Rehab Tips For Clinicians To Treat Gymnasts with Extension Based LBP – Part 5: Return To Training
Over the last two months I’ve been outlining my thought process for the rehabilitation of gymnasts with extension based lower back pain. The acute phase, sub acute phase, intermediate phase, and advanced phase of rehabilitation were Parts 1 – 4.
Before you dive in, if you want to learn everything I think about and do for gymnastics injuries, make sure to download the Gymnastics Medical Guide, and also if you are coaching be sure to download my Gymnastics PreHab Guide
Download SHIFT's Free Gymnastics Pre-Hab Guide

Table of Contents
Daily soft tissue and activation exercises
Specific 2x/week Circuits for Male and Female Gymnasts
Descriptions, Exercise Videos, and Downloadable Checklists

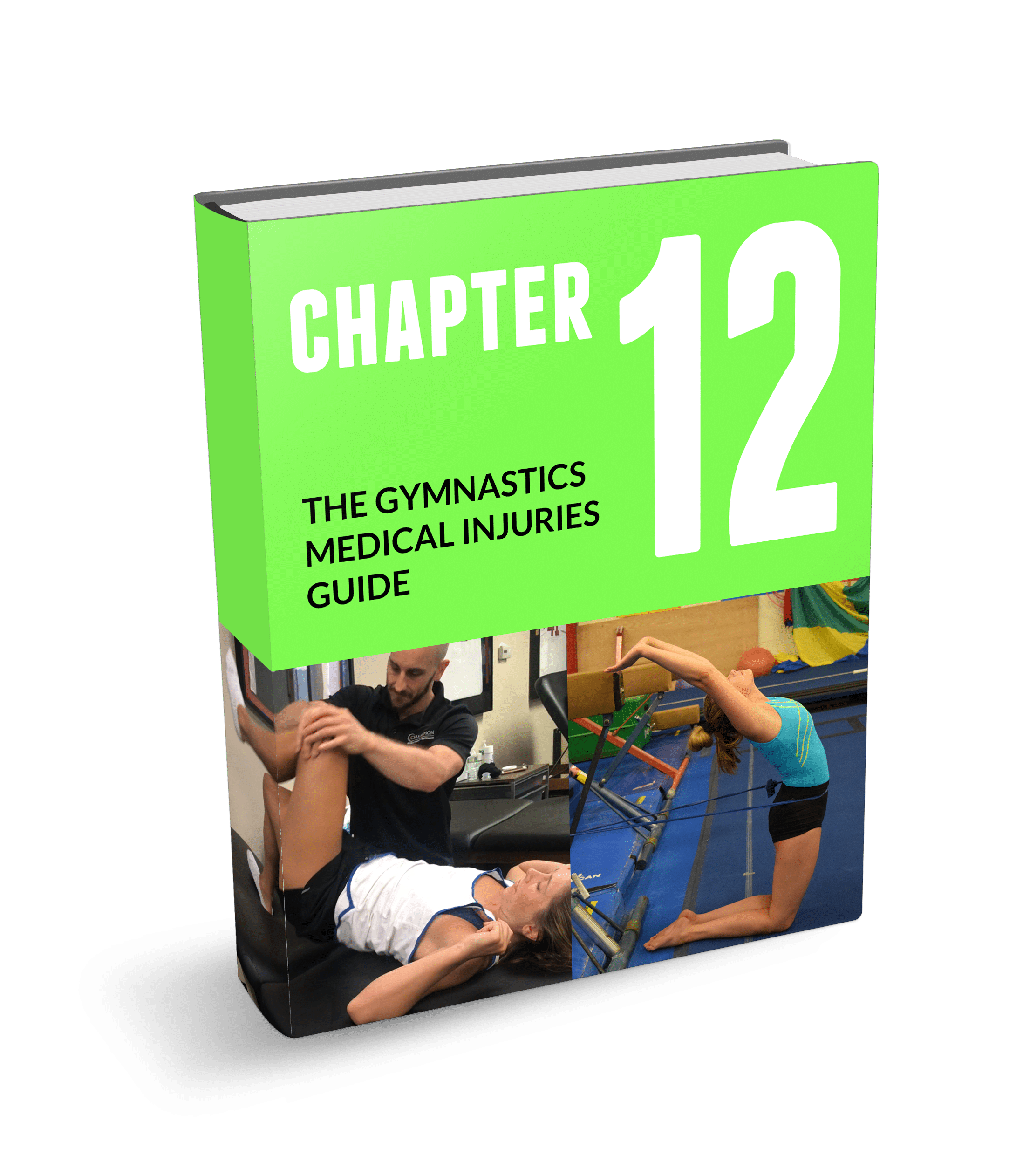
The Gymnastics Medical Injuries Guide
- Understand the most common injuries in male and female gymnastics, why they occur, and how to prevent them
- Read about the most current science on injuries and rehabilitation in gymnastics
- Get tips on the latest injury risk reduction and rehabilitation practices
We take our privacy seriously and will never share your information. Click here to read our full privacy policy.
In this Part 5 conclusion, I want to cover what I think is the most crucial part of rehabilitation, the return to gymnastics training phase. I feel team communication, objective exposure plans, a gradual progression of forces, and training variability are keys to a dramatic reduction in re-injury risk and overall increase in performance post injury.
The Importance of Team Communication During Return To Training
I can not stress enough how important communication between parents, gymnasts, rehabilitation specialists, doctors, strength coaches, and gymnastics coaches is. The best rehabilitation / coaching program can quickly get derailed by a lack of open communication between all team members. I have unfortunately seen this with my own gymnasts but also many parents, gymnasts, patients, and coaches who tell contact me with questions on injuries. There is often a large disconnect between all people involved.
Rehabilitation specialists must be sure the gymnast has proper extension and landing movement patterns, as well as make the best attempt to exposure them to high level strength and conditioning type programs in rehab. Any follow up testing or discharge from a doctor in terms of medical imaging for bone healing or growth plate normalization should also be clear. Healthcare providers must also use proper functional testing and higher level screening in the clinic. I have my own criteria of testing the includes plyometrics, fatigue protocols, the FMS, and other gymnastics specific tests. The coach must ensure all of these things transfer to training.

Any indication of soreness or pain during the first weeks must be reported by the gymnast. General muscular soreness from reconditioning is expected, but it should resolve with rest days and the gymnast must know pain (+ stork, midline sharper pain, etc) vs soreness. Should this occur everyone must take a step back to analyze why pain may be present. Parents must be alert for changes in the gymnasts status, as they are generally the one who see the athlete the most on off hours of the day. Coaches must be the ones who ultimately allow (or don’t allow) the gymnast to do certain things.
A very important point, gymnasts often feel out of place or pressured to work out when returning back to the injury. They are usually on limited practice schedules to heal their injury, but do not want to be viewed as “being lazy” or worse being viewed as a “wuss” not working out all practice. Coaches, the gymnast, and parents must understand that they have limitations and not push the athlete too soon. Healthcare providers and coaches should take time to outline what the gymnast should be doing if they reach their given assignment around limits from the rehabilitation exposure plan. I have gymnasts spend extra time on their home exercise program, event basics, drills, conditioning, flexibility, metabolic retraining, and other activities so they do not feel out of place. The more coaches and gymnasts get on the same page, the better for everyone and the better reduction in re-injury risk. This leads to the next two points.
The Importance Of Slowly Progressive Skill Exposure
From here, we must recognize that certain hyper extension skills are more demanding on the recovering lumbar spine. I add in new things weekly pending there is proper recovery days off in between and no increase in symptoms. All in all it usually takes 8-10 weeks depending on the level of the gymnast, reconditioning level, fatigue resilience, response to training, and their gymnastics skill profile. In terms of where to start, my skill exposure generally follows this based on symptoms. At some point I will objectively quantify this and hopefully have more research on spinal force exposures to use.
- Re-introduce basic flexibility and conditioning (no impact or hyper extension skills)
- Non impact/hyper extension basics and drills on floor, vault, beam, bars
- Tumble Trak and Trampoline light impact basics without forceful hyper extension (jumps, handstand pops, tramp jumps)
- Soft surface floor, beam (floor lines), and vault drills without forceful hyper extension skills
- Reps of partially unloaded extensions using spot, barrels, etc as first exposure, alternating with rest days
- Tumble Trak and Trampoline extension skills with proper extension patterns and
- Light swinging basics on bars, casts, and shaping
- Impact Jumps/Leaps/Dance beam and floor (no hard tumbling or dismounts to hard) with proper landing patterns
- Tumbling to pit, bar/beam Dismounts to mats in pit, and yurchenko drills like with uphill resi
- Hard surface tumbling, vaulting, and beam with proper extension and landing patterns
- Tumbling to mats, dismounts to mats, yurchenkos no flipping, beam dismounts to mats and low/medium beam series (proper landing form is essential)
- Full impact tumbling, swinging bars, high beam series, full vaulting

The Importance of A Periodized, Objective Interval Plan
Along with this I feel it’s crucial that a detailed, structured, and periodized hyper extension plan is made for the gymnast returning back to gymnastics. A healthcare provider should create it, a gymnast should understand/follow it, and a coach must reinforce it. I have seen many gymnasts who feel great and dive into training way to fast with no awareness of volume/density/recovery. I think a structured plan with gradual increase in intensity/volume can help reduce the risk of re-injury.
I create the initial return to gymnastics training based off many factors including
- Injury severity and time out of training
- The gymnast’s skill training profile
- Their competitive level
- Their age/developmental level
- The days and hours per week they train
- Their time of season, short term and long term goals
I have written before on understanding the difference in a gymnast’s skill profile, and how that greatly impacts what injury they might be at risk for. Compulsory gymnasts have a relative standard number of hyper extension skills, but as we move into optionals the number/density can vary significantly (Shaposh/Ray vs Geinger, Yurchenko vs Tsuk, BHS layout Stepout vs Back Tuck, etc). I strongly suggest healthcare providers talk with gymnasts to map their skill profile, then make an objective interval plan for them to follow on adding back in hyper extensions through the week.
As a mock example, here is a hypothetical extension interval plan I may make up for a level 10 who has a heavy hyper extension skill profile, has worked their way pain free up the skill introduction above, and is looking for full weekly practice return. I feel this helps to gradually exposure and recover healing tissues, helps the gymnast focus on quality of extension movement when getting back into training, and and helps progressively build motor control variability in the extension patterns with fatigue resistance during the day/week.
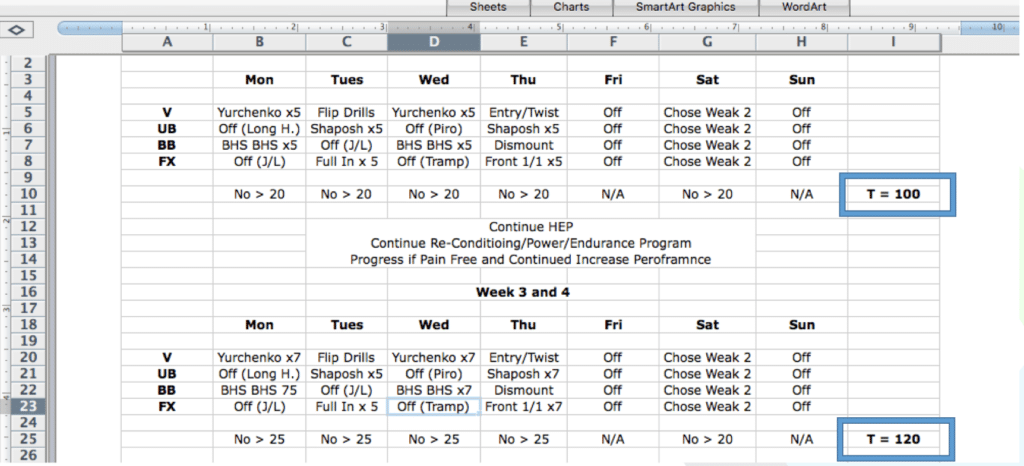
Take note of the “no > than ___” number that I put in to account for all drills, timers, warm ups, and so on. Also note the importance of no increase in pain before moving to the next stage, the slight increase in total numbers per week, and how when adding 3 vs 2 events in the numbers drop down to less per event. I use the last day of “chose weak 2” to have some focus on the most needed skills. due being a coach and knowing that importance. This may be tough for gymnasts and coaches to put the brakes on, but quality over quantity is important here. Again, just hypothetical as it must be completely individual and injury dependent.
This leads to another very important point about global coaching and training design. Both for the person returning to sport from a back injury, and also the prevention of back injuries from starting, we must consider what type of training focus we have day to day. Rotating what events/days hyper extensions and landings are performed to not overload our gymnasts in a practice or on back to back days. This is in order to hit every type of skill category (dismount, leaps/jumps, series for example on beam) and also alternate days of hyper extension loading. For example, here is what I outlined for our summer training program in relation to event focuses aligned with strength days to make sure we weren’t overloading our girls.

Concluding Thoughts
So hopefully within this posts I touched on concepts members of the multidisciplinary team can use for the optimal return to sport following an extension based spine injury. Obviously this series can not cover all the points as well as cover everything in return to sport. The concepts of formal periodized strength and conditioning for gymnasts could go in perfectly here, but I am going to save that for another time as it deserves much more depth and explanation. For now, I hope that everyone has found this series helpful. Best of luck,
Dave Tilley, DPT, SCS