Helping Gymnasts with Severs: 5 Steps To Reduce Pain and Get back to Training
Severs Disease, which is inflammation of the growth plate of the heel, can be one of the most frustrating things for gymnasts to deal with. Commonly referred to as “growing pains”, this overuse injury can substantially limit training, competition, and daily life. It is caused by a combination of high-force landing skills, high repetitions, and rapid growth spurts.
When you combine these factors with the reality that young prepubescent gymnasts have open growth plates that are softer immature bone areas that aren’t quite capable of handling the pulling force sof tendons, inflammation and pain can quickly start.
As someone who has treated 100s of gymnasts for heel pain, I wanted to quickly share what it is, and how to help. That way parents, medical providers, and coaches can find a quick resource should it come up.
Before I dig in though, if you are someone working in gymnastics who wants to learn about back pain, achilles issues, elbow OCD, and tons of non medical gymnastics drills, skills, and strength exercises, be sure to sign up for the 2023 virtual SHIFT Symposium we are hosting in June! This is going to be a monster 3 day event with 30 speakers and almsot 30 gymnastics lectures. I promise you will not want to miss out. Learn more here!
Table of Contents
1. Reduce Jumping and Running Forces
First and foremost, it’s important to understand that rest is essential when dealing with Severs disease. It’s frustrating, but there is no way to get better without allowing the bone to calm down. Severs disease is one of the most painful things someone can go through, and not resting properly will only delay the ability to get back to training safely.

I recommend a rest period of about two to four weeks, depending on the severity of the condition. Start with two weeks of completely no impact, followed by physical therapy and exercises, which we will cover below.
To help with pain, things such as compression sleeves on the calf, cold water soaks, elevation, massage, and anti-inflammatories (if recommended by a doctor) can also help manage the pain. Wearing properly fitting shoes that have a supportive lifted heel is also key, as it can take pressure off the heel and protect it from higher forces.
However, it’s important to reinforce that these things are not a substitute for proper rest, and will produce limited progress if an athlete is still participating in jumping, running, or other impact activities.
2. Light Soft Tissue Care & Stretching
During this rest period of two to four weeks, we can focus on calf and soft tissue work. Oftentimes, someone who is growing really fast can experience a lot of pulling on the calf complex, and it can pull on the Achilles, which then pulls on the growth plate. We want to do as much as we can to maintain calf and ankle flexibility during this time.
Foam rolling the calf on each side for 60 seconds, doing some lacrosse ball work on the bottom of the foot, and light stretching can slowly get some of the calf muscles to stretch and calm down.
Be sure not to stretch too hard during the acute phase when someone is experiencing a lot of pain. Instead, slowly reintroduce a little bit of stretching and flexibility work every single day for 30 to 60 seconds. These can be done daily to tolerance.
3. Rebuild Ankle Strength
After the first two to four weeks of rest and soft tissue care, we can start slowly loading the ankle under the guide of a medical provider. This is where calf and shin strengthening exercises come in, such as seated calf raises and standing calf raises. While its ideal to get to an elevated calf raise use weight, athletes can start on the flat ground and without weight first, and possibly try two legs instead of one. Tip toe walks are also useful for high relive strength.
It’s best to find a weight and duration that creates just enough soreness to feel the exercise working without actually worsening the pain. I recommend doing two to three sets of ten with a one-second tempo, about three times per week.
In addition to the calf raises it’s also crucial to incorporate some shin work. Often, the shins are not strengthened alongside the calves, which can lead to further problems down the line. I suggest doing standing heel lifts, leaning against a wall or off a stair.
4. Rebuild Leg Strength
During this loading phase, we want to make sure we are also addressing the entire leg. The stronger someones legs are, the more we can deload the ankle during jumping, landing, and sprinting movements. If we only focus on the ankle, and neglect the entire leg, we might hit speedbumps during the next phase of returning to impact.
We want to make sure we are hitting all types of movements. Exercises I tend to use are split squats, step-ups, hip lifts, and RDLs.
These can also be done 2-3x/week along side the ankle exercises above.
5. Return to General Plyometrics Slowly
After six to eight weeks pain levels should be lower and athletes should be tolerating moderate amounts of strength work. After this, and before returning to sports and high-impact activities, it’s essential to slowly reintroduce basic plyometrics, such as jumping and landing.
If someone can’t tolerate basic jumping and landing, they won’t be able to handle sprinting and other high-impact activities in gymnastics or other sports. I like to start with pogo hops, scissor hops, in and out hops, as well as jogging, skipping, side shuffling, carioca, and mini hurdle hops
These usually get someone to about 300 ground contacts, and with two to three days in between we can monitor symptoms. These can be progressed over two weeks.
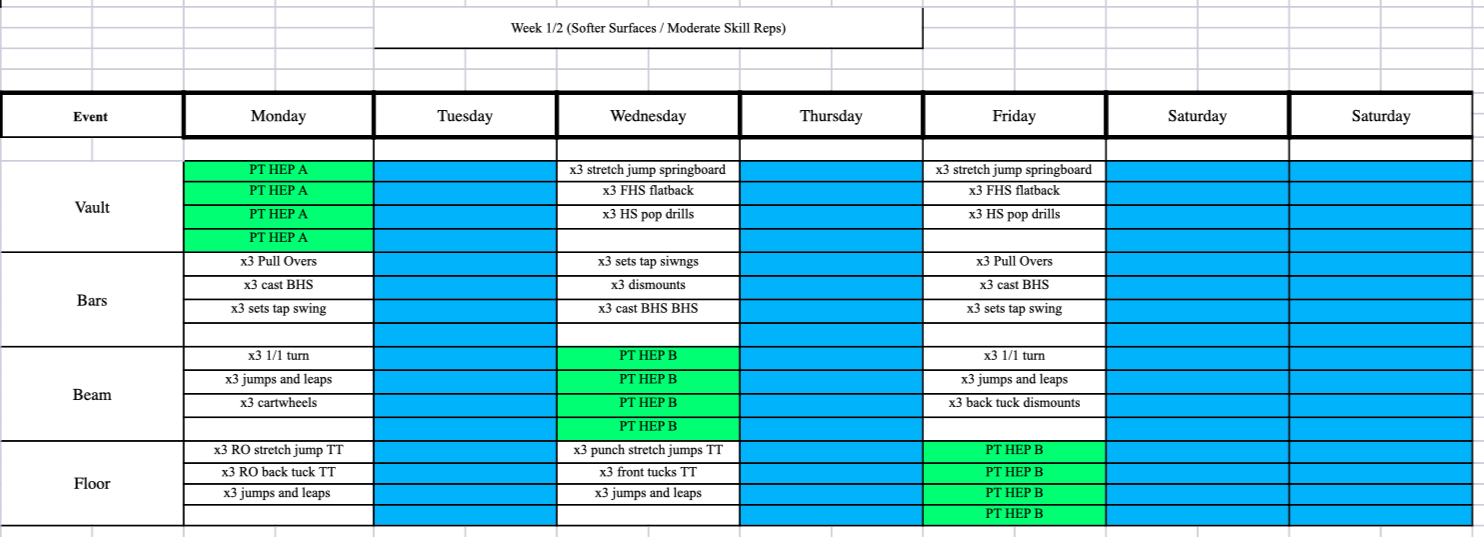
After this goes well, we will slowly add back two weeks of soft impact in gymnastics-specific settings. It’s crucial to start with basic movements before moving on to more advanced exercises. For example, we can start with jumps on a trampoline or tumble track, which are more forgiving than hard floors. A few sets of 10, alongside the plyometrics above, are good two to three times per week.
At this time, I also like to add in-depth drops and broad jumps to start adding more force to the heel.
After this entire progression is done, usually at the eight to twelve-week mark, athletes are feeling better and ready to return to sports pending that doctors and rehab providers have cleared them.
Concluding Thoughts
Although frustrating and requiring patience, there is definitely hope for those athletes struggling with Severs. The keys to success are
- Addressing problems early and head on, with great communication
- Properly resting from impact and allowing bone healing to relieve pain
- Progressing local ankle and global leg strength
- Progressing general plyometrics first before gymnastics-specific impacts
- Progressing from soft to medium, to hard surfaces gradually over two to four weeks when returning
Again, if you are a medical provider or coach working in gymnastics who wants to learn everything about growth plate injuries and other common problems like elbow OCD, back pain, shoulder instability, and more be sure to grab tickets to the 2023 SHIFT Symposium.
I hope that was useful for everyone out there! Best of luck
– Dave
Dave Tilley DPT, SCS
CEO/Founder of SHIFT