A Brain Spill on Mechanical vs Neurological Effects in Physical Therapy (Part 2)
Stuff That Actually Relates to Treating People
Based on all the really geeky thoughts I had and research articles I talked about in Part 1, here are some more clinical based thoughts on the mechanical vs neurological debate. Remember, just thoughts and opinions based on all the stuff I read.
- Manual Passive Range of Motion – Hands on passive motion may act as a huge barrage of afferent input to the nervous system. Joint receptor stimulation, proprioceptive input, and other sensory feedback may be a very positive mechanism following injury. Both in terms of your hands on the person and also the ligament, soft tissue, and capsular feedback detected. Is this range of motion reducing threat associated with the area by introducing some non-nociceptive signals to the CNS? Maybe offering competitive non-nociceptive input does truly allow tone modulation and relaxation of the soft tissue guarding the joint to prevent motion.
- On the other side of the coin, maybe this passive range of motion has a very mechanical based effect allowing for the involved tissue to regain it’s tolerance to stretch or passive tissue strain tolerance against movement. It may also create a positive tissue environment by generating tension and compression the person is unable to do themselves. If someone suffers nociception overload/inflammatory peripheral sensitization, the CNS may down regulate or redistribute activity to allow proper rest of that area. Maybe the manual motion may help replicate some of the mechanical signals that are normally created to with volitional muscle activation. It could also be synovial fluid hydration to cartilage surfaces and blood flow may also very much be occurring to help promote tissue remodeling.
- A lot of more neural side of the fence people knock soft tissue/ passive work for fear of patient dependency or wasting time, but I think that’s being a little tunnel visioned. That being said, all soft tissue only people do can benefit by doing some homework on the value of what heavy loading can do.
- This is so long that the passive range does not excessively stress healing tissue (certain cartilage surgeries in the knee as well as certain rotator cuff repairs and labral surgeries in specific ranges). As supported in some stem cell, PRP, and other mechanical model papers, the tensile or compressive forces may be a very important stimulus to promote new tissue growth through mechanotransductive pathways on a cellular level. When applied properly this shows an important overlap of knowing mechanical forces on the joint compounded with possible neural effects, as well as joint biomechanics.
- Connecting this to the mechanotransduction and cytoskeletal model, a recent Ingber paper describes the cellular network (outlined as an unconstrained structure) as needing “prestress” in order to maintain it’s shape and solidity. I think this is huge. After an in-depth mathematical outline, he summarizes with
- “stability of the unconstrained structures cannot be provided by elasticity of their structural members and thus they need prestress to maintain their shape and solidity“
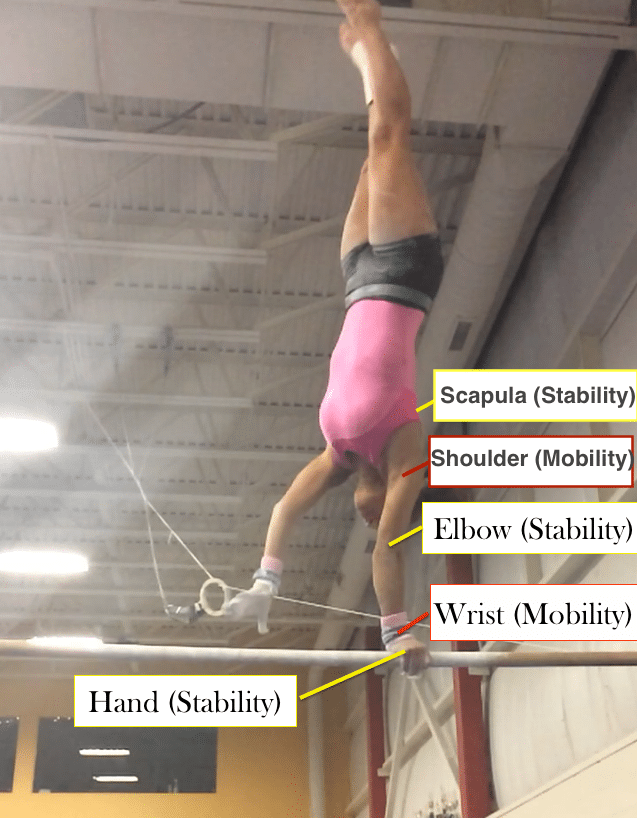
- Intuitively for me, I would question how this prestress is generated in the muscular system. Brainstorming on this topic helps fill in the black hole that “stability training” sometimes creates. It only makes sense to me that this ability to prestress the cellular cytoskeletal structure and allow it to transmit mechanical forces comes from neurological influences. Motor control and other neurobiological research (Latash and Zatsiorsky come to mind) discuss how anticipatory motor programs, reflex arcs, and conscious/subconscious mechanisms regulate neurally driven muscular tension. These neural mechanisms have also been outlined as a very important feature to complement serial elastic passive tissue elements in plyometric movements common in sports/life.
- “Bigger Picture” Type Treatment Example – Dynamic stability work of the hip/shoulder joint to train rotator and cuff to co – contract against perturbation….As the rotator cuff and other musculature of the hip/shoulder blend into the joint capsule does this connection of training neurological control through manual perturbations link to mechanical carry over of “stability” through tensional prestress. Neurological control may create mechanical tension through the system via prestress and mechanotransduction, thus leading to better maintenance of the humeral/femoral head to prevent micro-instability and passive joint or labral overload. A very hard theory to validate, but seems intriguing.
- Is this a possible supportive mechanism to why so many more lax individuals (gymnast, baseball, swimmers) have instability issues in the shoulder/hip. Maybe it is due to the increased compliance of ligaments and capsules not being able to efficiently transfer mechanical prestress signals through the tensegrity based cytoskeleton that is highly dependent on mechanical tension to create stability. Some laxity tendon research has outlined these individuals with more collegen, and even sometimes lacking proprioception for tensional feedback and reflex arcs detecting stretch. If this stretch signal is missing with more passive tissue laxity, it may be negatively affecting the tissues ability to create prestress and tension to create dynamic stability.
- By training high-level dynamic stability, increasing strength, and training neurological control can we help them compensate for this lack of inherent passive tissue stiffness and train the athlete to protect the area being overloaded? Again, theory for why conservative PT may help many clients. Often times people get living or playing sports with RTC tears and hip /shoulder SLAP tears. We can help put out the initial injury fire and then enhancing their joint protection through strength/dynamic stability work, along with monitoring training load closely and considering sports biomechanics.
- Also, this highlights the crucial role strength and conditioning from early age plays in this more lax population. This may create a very important overlapping training principle for neurological control and mechanical stability under very high-stress conditions (jumping, throwing sports, hanging traction force, etc). This may help explain the pathway and need to develop the neurological reflex or tuning the afferent receptor organs of the muscular system so that prestress and tensioning can exist in the pretense of huge forces in sport/life.
- I really have no answer to this above theoretical construct, but in my mind, it outlines the crucial overlapping of neurological influences to this very mechanical cellular cytoskeletal-based theory. The role of the central nervous system to act on very mechanical based system components is huge. Moving the other direction, the afferent mechanical signals (tension, compression, force transfer through cytoskeletal scaffolding) being interpreted and processed by the nervous system for movement goals is also huge. I would argue this matters both in the manual therapy and exercise domains. They are way more overlapping and similar than different.
- These were thoughts triggered by watching gymnastics swing super hard and land with enormous forces going through their hips and shoulders, only having milliseconds and the training or pre-programmed motor patterns to utilize. This combined with the need to increase tissue capacity through formal strength principles to tolerate this huge impact repeatedly spark the overlapping neural/tissue level effects both locally and globally in the body.
General Concluding Thoughts
- I could be completely wrong in these ideas and theories, given I clearly am no expert in cellular biophysics or neurological motor control. Honestly, I hope that I am wrong about some things and people reach out to me with constructive ideas so I can continue to narrow in my thought process. It still has to move from wide-ranging and theoretical, to more concrete applications that help people.
- A lesson I have picked up from learning from different people/systems is the important concept that no one way rules the road. As I think many would agree, when new concepts emerge our pendulum tends to swing very far to one side, then often people reel things back in down the road. I think this exact concept has happened with manual therapy and the mechanical vs neurological debate. To be completely honest, I believe there is huge value in considering both concepts.
- Not to mention, the evidence is emerging about overlapping theories of why certain manual therapies/self-manual therapies work. Take for example the recent collaborative work on tendinopathy from BJSM or overlapping work of Paul Hodges, Stuart McGill, Lorimer Moseley, Shirley Sahrmann and others in Paul Hodge’s 2015 Spine book. It ultimately always comes down to using your clinical rationale and judgment to help the individual person in front of you, based on how they present and their beliefs about what will improve their current status.
- From the neurological point of view, I have absolutely worked with many clients who present in a way that will favor more the of the non-mechanical approach to their treatment. They may have misconceptions about manual therapy and “no pain no gain”, they may be extremely sensitized from their recent lower back flare up, and may also have been given misleading information about how awful their X-ray or MRI looks. Sometimes a mechanical approach can scare these clients even more.
- When I say “low back pain”, I don’t just mean the average general population client with chronic lower back pain most people jump to imagining. I certainly have had high-level athletes with the same acute flare up of lower back pain that need someone to help them calm down a little. Sometimes they jump to conclusions that their SI joint is dislocated or that they fracture their back. Sure enough, they did just fine with reassurance and a lighter more nonmechanical approach to things in those first few days. It’s all about having some emotional intelligence in the moment and reading the person in front of you, not just blindly going by what the text book says orthopedically.
- On the other side of the fence, we have to consider sport specific muscular adaptations to supra physiological loading or repetitive overuse in the same pattern (throwing, running, swimming, etc). The bias towards neurological vs mechanical effects with more pressure and intensity may be shifted based on the population you see regularly. This may be a situation where manual therapy and a more mechanical approach is very applicable to maintain the soft tissue extensibility seen with regular overuse. This is even more so when considering biomechanics of the sport and what may have created tissue overload in the first place. Specific sports will have specific injury risk based on the mechanism. The gymnasts I work with won’t likely have to worry about internal impingement from throwing where as the baseball players Mike and Lenny work with probably don’t need to worry about hip micro-instability during end range hyper extension. Their injury may have more true mechanical and load based adaptations that if are not maintained, can create issues in movement quality or local tissue overload.
- I think this speaks to the role of soft tissue quality maintenance and proactive or maintenance care. Clients have to understand we aren’t only here for them when they are hurt. If you need a specific range of motion overhead, but lose it overtime due to repetitive training or loading, the gap that exists between what you need and what you have may become a huge issue creating tissue irritation in the long run. The competitive season of gymnastics is brutal, and the group of maintenance care athletes I have currently are doing really well.
- The same goes for legs and squatting volume, throwing, running, and so on. One of my favorite Mike Reinold philosophies is “I want you to be you when you pick up a ball, not more than you and not less than you”. He hits the nail on the head for this concept. This plays into the bigger picture of training load monitoring and acute vs chronic work load ratios, but that is a much bigger discussion for another time.
- It’s impossible to think that only neural influences/effects will lead to success. On the same side, it’s impossible to think only mechanical based approaches are the way. It is all based on the client in front of you, their injury/complaint, goals, and being sure we use clinical reasoning and available research for what that person may need. If a patient comes in super acute, has signs of peripheral/central sensitization (or to be honest is just really worked up) an easier and more neurological approach may be warranted. On the other side of the coin, there are times when more force is necessary to not only gain motion and prevent scarring (post-operative).
So, that is all for now on this blog post series. I hope people have enjoyed reading through some thoughts and have created plenty of their own. Happy Holidays!
Dave Tilley DPT, SCS