Back Pain in Gymnastics – A Complete Guide
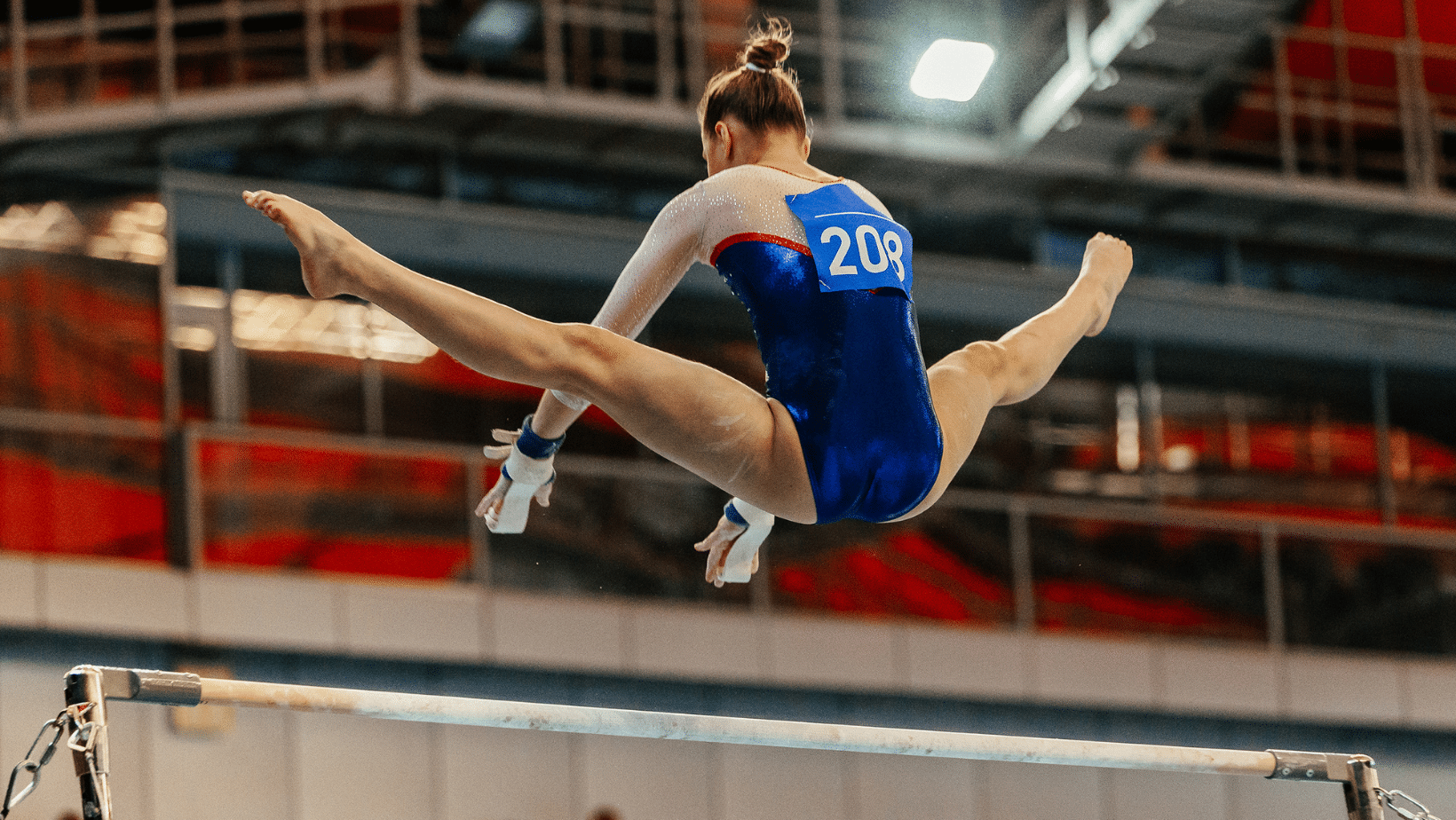
Lower back pain is something so many gymnasts struggle with. Depending on the research study you read, between 71% – 96.6% of all the injuries reported are to the lower back. Most literature puts lower back pain as the second or third most common injury in gymnastics, just behind ankle sprains and knee injuries. Sadly, knowing the culture of gymnastics and the stoic nature of many athletes, I believe the research doesn’t accurately reflect just how bad the rates and severy of lower back pain are in gymnastics.
As a former collegiate gymnast, and a current gymnastics coach/Sports Physical Therapist specializing in gymnastics, I know that thousands of gymnasts suffer. They think their back pain is “part of gymnastics” or are told that there is nothing they can do until they quit gymnastics. While there are some times when this situation might come up, the reality is that the majority of lower back injuries do not require someone to completely stop gymnastics. There are many different training changes, skill modifications, strength and conditioning, and cultural issues that can be tackled first to try and make progress.
It is crucial that a gymnast get the proper evaluation, and accurate diagnosis, for their back pain. A common misunderstanding in the medical and gymnastics world is that gymnasts only get pain from back bending. This is very misguided. It is true that back bending does cause lower back pain in many gymnasts. But, there are also many other types of forces and skills in gymnastics, that create quite different subtypes of lower back pain. I have treated 1000s of gymnasts for back pain in my career, and can tell you that forward, impact and traction-based lower back pain are also very common.
Due to how many gymnasts struggle with back pain, and how many medical providers ask me about how to help them, I wanted to create a “mega” blog post and podcast resource for people. My hope is that by taking the time to really break down everything in-depth, parents, medical providers, and anyone else working with gymnasts, can have this blog post as a reference.
After this short introduction, I will start by outlining how common back pain is in gymnastics. I will then review some of the biggest factors that might be most important to understand as to why these lower back injuries occur. Following this, I will break down the basic anatomy of the lower back and the most common injuries we see frequently in gymnasts.
Then, I will walk people through the 4 main phases of injury rehabilitation, share the exact exercises/approaches I use with gymnasts, and talk about returning to sports safely. To conclude things, I will discuss some ways that we can work together to reduce the risk of back injuries in gymnastics and offer help for people who may be really struggling with ongoing pain.
Table of Contents
In-Depth Courses for Gymnastics Coaches and Gymnastics Medical Providers
Before going down the rabbit hole, I know that many people want a “step by step” instruction guide for fixing gymnastics back pain.
If you are a gymnastics coach, I have 40+ of webinars, handouts, and discussion boards inside our online gymnastics education group The Hero Lab. We cover everything from flexibility, to strength, to culture, and more while getting access to monthly “Office Hour” live Q&A’s.
For Gymnastics Medical Providers, I have an 8.5 hour PT/AT CEU approved course where I will teach you exactly how I treat gymnasts for hip, lumbar spine injuries called Evidence-Based Evaluation and Treatment of Back Pain in Gymnasts. You can check them below out if that fits your fancy.
If you prefer to listen to this in podcast form or watch it in video form, you can check those out here!


How Common is Lower Back Pain in Gymnastics?
To first understand how common back injuries are in gymnastics, let’s review some epidemiological studies. These are studies that look at the rates and prevalence of certain injuries within different areas of gymnastics.
- O’Kane 2011, 96 Club level gymnasts Level 4-10
- 8.8% of acute and 18% of all overuse injuries
- Fett 2017, 32 German elite gymnasts
- 93.8% lifetime prevalence, with 68.8 3 month prevalence
- Kerr 2015 in NCAA Gymnasts, 11 programs with 418 injuries over 5 years
- Low back pain was 13.4% of all injuries (but categorized as ‘trunk’ injuries
- Kolt 1999 of 64 elite and sub elite gymnasts over 18 months
- Low back pain was 14.9% of all injuries, 2nd most common
- Salun et al 2015, 21 year study of 3681 injuries from elite/intermediate/novice level
- 11.1% overall incidence, 400 back injuries total
Why Is Lower Back Pain So Common in Gymnastics?
High Back Bending Skill Repetition

While I mentioned there are many subtypes of lower back pain in gymnastics, the reality is that backward bending (or extension) is by far the most common trigger for pain. When you look at the sport of gymnastics, it has a very high amount of extension-based skills that are done repetitively. Bridges, front/back walkovers, front/back handsprings, arch taps for giants or release moves, arch taps for Moys and ring giants in men’s gymnastics, Yurchenko vaults, jumps and leaps, and so on. Even in the lower levels or non-competitive side of the sport, it is very easy for a gymnast to stack up thousands of backbends per month. These skills are not inherently ‘bad’ for gymnasts, and I don’t want to scare anyone off from doing the sport. In the proper dose and context, with the right training, there is no need to worry.
That said, as I will break down extensively in the sections to come, there are certain structures in the lower back like the facet joints and the pars interarticularis that become stressed with these repetitive motions. If left unchecked, and not properly managed, it can easily create a situation where back pain starts. Next to this, if a gymnast is not taught how to backbend properly, and is not properly coached/monitored to protect their lower back, the poor technique might also create excessive stress and possible pain.
High Back Rounding/Impact Repetitions
Alongside the repetitive back bending motion, gymnastics also requires an enormous amount of rounding (or flexion) and impact (or compression) repetitions. Skills like front/back rolls, front/back tucks, kips, in bar skills like toe ons, peaches on parallel bars, yamawaki’s on rings, jams on high bar, and more all require very deep pike positions and rounding of the lower back. These motions can sometimes irritate the muscles, joint capsules, discs, and nerves of the back during such high forces.
In a similar context, many different tumbling skills, vaulting skills, jumps/leaps, and dismounts put massive numbers of impacts on a gymnast’s spine. These impact forces are enormous, ranging from 15.9-18x bodyweight. If not properly trained for and approached slowly, it can create irritation of muscular tissues, the bones of the back, nerves around the spine, and something called the endplates.
Just as with the above section, these things are not inherently bad for gymnasts. But due to how often they occur, and how often gymnasts must do them to get skill progress, we have to be extremely calculated in how we approach our training with kids. If we don’t have a science-based, specific training program, these repetitions can add up fast and lead to possible back pain.
High Force Skills
While the repetitions of skills are by far one of the biggest factors for why a gymnast may develop lower back pain, we can not deny the reality that the forces that gymnastics puts on the lower back of a gymnast are enormous. In an effort to help condense some of the research around this (all in refernces below), here is a list of forces that have been recorded on the spine during gymnastics skills.
- Shearing forces during front tuck on floor: 1.4x body weight
- Shearing forces during back tuck on floor: 2.2x body weight
- Shearing forces on L5-S1 during Tkachev release rap: 4x body weight
- Shearing forces during downward ring giant swing: 6.5 – 9.3x body weight
- Take off compression forces on floor: 6.5x body weight
- Average compression during landing: 11.6 – 14.8x body weight
- Dismount shearing forces at the L5/S1 disc: 3.5x body weight
- Maximum compression forces during flexed landing: 40x body weight
These forces really are staggering. We don’t need to be terrified by them, but more so respectful and aware of them. These skills, and many others, can all safely be trained and performed. The key here is to make sure that proper technique, progressions, workload management, and strength/physical preparation are used to help manage risk.
Limited Shoulder, Upper Back, Hip, and Ankle Flexibility

It is crucial that a gymnast have enough shoulder, upper back, hip, and ankle flexibility if they want to reduce the risk of lower back pain as much as possible. More than any area of the body, having enough flexibility above and below the lower back to ‘spread the bend’ out, or help land properly, is key.
Let’s use back bending for example. I tell gymnasts I treat for back pain, when you do a large back bend motion in a back walkover or back handspring, we want to share that lead to as many places in the body as possible. Ideally, the shoulders, upper back, lower back, and hips all bend about 25% so that no one thing gets overloaded.
But say you have some limited overhead shoulder/upper back flexibility and limited hip-opening flexibility, due to natural growth spurts and the repetitive training that happens in gymnastics. The muscles in the shoulders (lats and teres major) and hips (hip flexors, quads, groin) can easily become stiff and lack flexibility. Now we have a situation where maybe the shoulders are only doing 10%, the upper back is only doing 10%, and the hips are only doing 10% of their opening instead of the ideal 25%. This means that the lower back must work extra hard and do 70% of the work to pick up the slack from the other areas.
Given the high repetitions of back bending and the high forces on the lower back during those skills, this may become a problem quickly. That means for all the back bending type skills, a gymnast is constantly overworking their lower back and might put too much stress on the muscles/bones of the spine. The same concept can apply to ankle flexibility in gymnasts and back pain. If a gymnast lacks the ankle flexibility to properly absorb high force landings/dismounts, they may put excessive force into their lower back, and create pain. For this reason, it is absolutely crucial that shoulder, upper back (thoracic), hip, and ankle flexibility is screened for and worked on in gymnasts.
Gymnasts Being Young & Pre Puberty
Another tough pill to swallow – the majority of athletes training in gymnastics are children. Despite ages trending upward for the world and Olympic teams, the vast majority of people competing in gymnastics are under the age of 16. They are young kids, who have yet to fully develop physically or mentally. This means, according to great research and textbooks, they are nowhere near their peak strength, power, or cardiovascular capacity.

Not to mention, their growth plates are wide open and very vulnerable to injury. If gymnasts are not developed enough or lack the physical preparation to protect their spine joints and open growth plates, injuries muscular spasms or stress fractures might surface. It’s crucial that young gymnasts have the core, hip, leg, and general strength to help buffer these high forces going through their lower back joints that are not fully formed yet.
Gymnastics is a very unique sport where very young kids ages 8-12 are asked to perform very high force skills, in high amounts, and are training 20+ hours per week in some situations. In some areas of the sport, particularly those trying to get on the pre-elite/elite or NCAA track, it can create a difficult time period where pre-pubertal athletes are training high force skills, in high repetition, well before their bodies are physically or mentally capable of handling it. This is where expert coaching, training plans, and pacing comes must be a priority.
Lack of Science-Based Strength & Conditioning Methods
This is something that applies to all gymnastics injuries but in particular low back pain. As mentioned, the forces on the lower back of gymnasts are massive. If you look at the sports medicine literature, it’s clear that other sports use science-based strength & conditioning to help reduce the risk of low back pain. This includes evidence-based, progressive weight training using dumbbells, kettlebells, medicine balls, and barbells.
Based on great literature (more here, here, and here), it is clear that a properly done, properly coached, and properly progressed strength and conditioning program is beneficial for performance and reducing the risk of injuries. This includes a combination of both external weight lifting and bodyweight strength work. This type of training is huge to help build the core muscles, and the other dynamic stabilizers, to protect the ligaments, bones, and joint capsules in the lower back. Taking this one layer further, a lower/upper body strength program can be insanely beneficial to help absorb the very high forces that gymnasts experience during skills.

Despite the abundance of evidence, there is still a huge percentage of gymnastics professionals who feel that gymnasts should not be lifting weights. They fear myths and misunderstandings about weight training, believing that it will make gymnasts “bulky”, less flexible, and cause injuries. However, a closer look at the literature show this to be largely false, given the program is properly implemented and coached with an aim of improving explosive power. Even more so, it is clear that weight training is not only not dangerous for kids, but likely helpful in reducing injury risk.
As a result of this cultural barrier, many gymnasts do not get the adequate core/leg/arm strength and capacity needed to handle the high-impact forces going through their spine joints. Not to mention, they are putting a huge bottleneck on their potential to train and compete for high-level skills. Gymnastics is a sport based on explosive bodyweight power. The same thing that helps improve this power will also help mitigate the risk of back injuries, both overuse and acute. For more information about this topic check out this popular blog post I wrote in 2016.
Also, if you would like to read my “Ultimate Guide to Gymnastics Strength” – you can check it out here.
Improper Landing Techniques Still Taught & Used
Another huge change that must be made in gymnastics to reduce the risk of lower back pain injuries is a sport-wide adoption of using science-based landing mechanics. It is unclear whether this comes from a lack of education, an ‘old school’ mindset, or a desire to mimic the esthetic type landing seen in ballet or dance.
However due to this, many people in gymnastics still teach use, and judge, based on a landing position that is not supported by science to ideally help dissipate high forces. Many gymnasts still land with their feet together, torso upright, hips tucked under, and in a ‘knee’ dominant patterns that may shift more stress onto the back, knee, and ankle joints. In fact, it was recently shown in a study of elite gymnasts in the UK, that they tended to land with a ‘stiff’ landing pattern with an overextended lower back position.

This is in contrast to the suggested landing pattern, supported by enormous amounts of data, of a squat based landing that has the feet hip-width apart, knees tracking in line with the hip and feet, and the allowance of squatting to parallel depth so various musculature can be recruited to buffer forces.
Until this becomes the gold standard for teaching gymnasts how to land in practice and competition, we may continue to see high back pain rates. I recently gave big presentations to the coaches and judges in the NCAA about this topic that you can check out here.
Sport Culture – Early Specialization
One of the most important, yet most challenging, issues at hand is changing gymnastics culture. The last five years have clearly shown us that there are many dark corners of a gymnastics training culture that exist in “old school”, archaic methods being used. There has been a massive amount of scientific data published around early specialization (here and here), year-round training (here and here), strength and conditioning (here and here), workloads (here and here), that have yet to make their way into mainstream gymnastics training.
Early specialization, when an athlete chooses to only participate in one sport, is one of the biggest concerns. It is common to hear gymnasts being told they will ‘miss their shot’ if they don’t only do gymnastics from a young age. While I do believe that gymnasts, particularly those with high-level goals, may need to specialize earlier than most sports, asking a 6 or 7-year-old to only train in gymnastics and not experience other sports is asking for disaster.

There is great evidence that this is concerning for increasing the risk of burnout, overuse injuries from repetitive movement patterns, and that it may negatively impact their overall athletic potential long term. The majority of the literature suggests that 14 or 15 years old is ideal for specialization. With that in mind, I think that may be unrealistic for many gymnasts, and that 10-11 might be a better target.
But hearing about gymnasts specializing at 8 years old, as studies including one in the NCAA I was part of have suggested, is definitely concerning for all injuries. This is something our sport desperately needs to talk about and change to protect young at-risk gymnasts. While there is a large range of movements in gymnastics, the repetitive impact of only doing gymnastics from a young age might be a big reason so many lower back injuries are so common.
Sport Culture – Year-Round Training
Year-round training is another concerning cultural phenomenon that continues to persist in gymnastics. As with early specialization, there is an abundance of research across many sports (more here , here, and here) suggesting that athletes who train more than 9 months out of the year in a single sport are at elevated risk of injury and burnout. This has been well studied in baseball, which is a sport I’m fortunate my mentors Mike Reinold and Lenny Macrina were pioneers in alongside current studies like this.
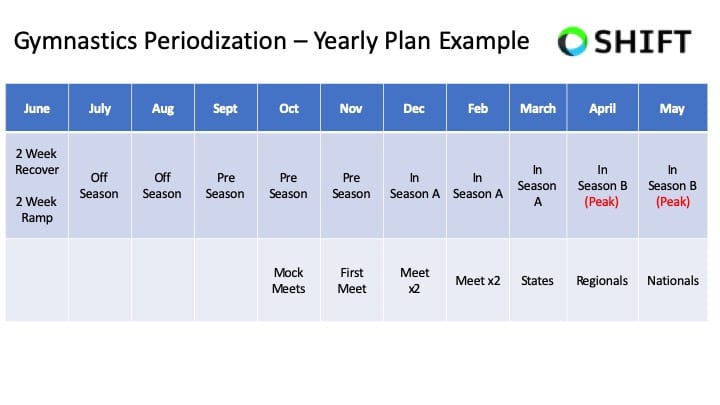
I strongly feel that creating relative off-seasons, using periodization, and utilizing cross-training are crucial for reducing back injury risk and optimizing performance. The reality of our sport is that there has never been a time when gymnasts followed evidence-based guidelines around recovery, offseasons, and science-based work to rest ratios.
My hunch is that remodeling our year-to-year approach, shortening competitions seasons, and giving athletes a relative off-season after their hardest meet, would yield massive improvements in health and performance. I think the COVID pandemic is a further support piece of this, where many gymnasts said that after 2-3 months off, they felt the best they have ever felt mentally and physically. I don’t think it’s wise to give gymnasts extended periods of time fully off each year (3+ months for example). Hower, 4-6 calculated weeks would likely be incredible for athletes, coaches, and parents.
Lack of Science-Based Workload/Wellness Monitoring Programs
Workload, athlete monitoring, and periodization are all areas of research that have become very popular in sports around the world. It is very common to hear about sports like soccer, basketball, and baseball utilizing specific workload tools to help plan and manage training volumes in athletes.
While there has been more conversation about workload management in gymnastics, the current approach still largely depends on a coach’s perception for decisions to be made. This was recently shown in Rhythmic Gymnastics but is likely the case in other domains such as artistic, trampoline & tumbling, and more.
The truth of the matter is that while there is some data in gymnastics forces, we still have a tiny fraction of what is needed to create evidence best training plans around impact and health. We have no idea what the impact forces on the back joint are for a Tumbl Trak, vs Trampoline, vs a rod strip, vs a new spring floor, vs an old spring floor, vs a spring floor with a sting mat for take-off or an 8″ mat for landings. By not knowing these numbers, and by not having a logical progression of forces over multiple weeks, we are essentially asking coaches to fly a plane without any speedometer or gas gauge. It’s insane, and a huge reason we continue to see so many gymnasts struggle each year.
If we hope to curb the rates of back pain in gymnastics, it is imperative that we look into better tools for external and internal workload tracking. Without knowing what the forces of different surfaces are on the foot/ankle, and how to keep a close eye on the training load gymnasts take, it’s like trying to fly a plane without any gauges or speedometers.
While this is evolving in gymnastics and is a field I’m actively doing research in (see below), the reality is we still have a long way to go. We desperately need research to be conducted on the different forces on the back joint during tumbling, vaulting, and dismounts. We also need better systems in place to monitor how athletes are responding to gymnastics-specific training. This will help us enormously to plan, track, and keep in touch with how gymnasts are doing.

Gymnastics Basics/Foundational Technique Sometimes Not A Focus
On the sport-specific side of things, it has to be mentioned that technology itself is a huge factor in injury risk for gymnastics. While there is not as much scientific evidence looking at different types of gymnastics skill techniques, it’s paramount the gymnasts are taught proper basics, foundational techniques, and progressions.

This is particularly true for the lower, where proper tumbling, vaulting, and bar technique is crucial. Gymnasts must be put through the proper technical progressions skills and events to make sure they are equipped to handle the high forces of skills. If these foundations are not set from an early age, and a constant focus as the gymnast progresses in level, it might create high-risk situations. Making changes here comes down to better coaching and education systems throughout the world, to share. the optimal technique and progressions to keep gymnasts as safe as possible.
Equipment Technology Progression
Lastly, there is no denying that the sport of gymnastics has become exponentially harder in the last 10 years as equipment technology progresses. The spring floor, the vaulting table, the trampoline beds, and other advancements have helped skyrocket the level of skills being performed. The double-edged sword here is that this also increases the average force the body takes.
While the landing surfaces and matting have also increased in their ability to protect athletes’ , the net increase in force is still substantially higher in today’s gymnastics environment. It also creates a small ‘ripple effect’ on the younger generations, where the nature of harder skills being performed means that more time, effort, and possibly starting to learn these skills at a younger age, also occurs. Coaches must be trained on how to use different equipment for proper progressions, and we also have to financially support gyms that need better equipment to keep athletes safe.
Basic Low Back Anatomy As It Relates to Injuries
I by no means am here to bore people with a dissertation in anatomy. But if we wish to make a change in the rates of back injuries, we must first understand the anatomy that contributes to those injuries. This helps to understand the nature of common injuries and leads us down the road of helpful strategies to reduce risk.
If you want all the scientific textbooks and anatomy references to look up, check out this textbook, this textbook, this textbook, this textbook, and these textbooks as well as some helpful research articles here, here, here, and here.
Layer 1 – Bones & Discs

Vertebrae
At the most basic level, the spine is a series of alternating bones and discs. The bones, referred to as vertebrae, are the main weight bearing structures that create the overall structure of the spine. There are 5 lower back vertebrae, referred to as the lumbar spine collectively. They are stacked on top of the lowest level of the spine, called the sacrum.
The main bone area of the vertebrae is the “body”. This is the surface that anchors the discs (more below) and also is a broad, flat surface made for weight-bearing. On the top and bottom of each vertebral body is something called the endplate, which serves as the anchoring mechanism for the discs. Special fibers called Sharpey’s fibers help attach the disc to these endplates to provide high levels of support.
Extending outward from the back of the vertebral body is a ring-shaped structure that houses the spinal cord, and also has smaller boney elements to create the lower back joints. This ring can be broken down into other boney structures known as the pedicle, the pars interarticularis, and the lamina.
Extending from this ring are the articular processes. Two transverse processes extend outward (one left, one right) and one spinous process extends backward. Additionally, two superior articular processes extend upward and two inferior articular processes extend downward. These upward and downward processes connect adjacent vertebrae with the processes. The two downward processes of one spine level connect to the upward processes of the spine level below it. This connection through articular facets creates the main spine joints, called facet joints.
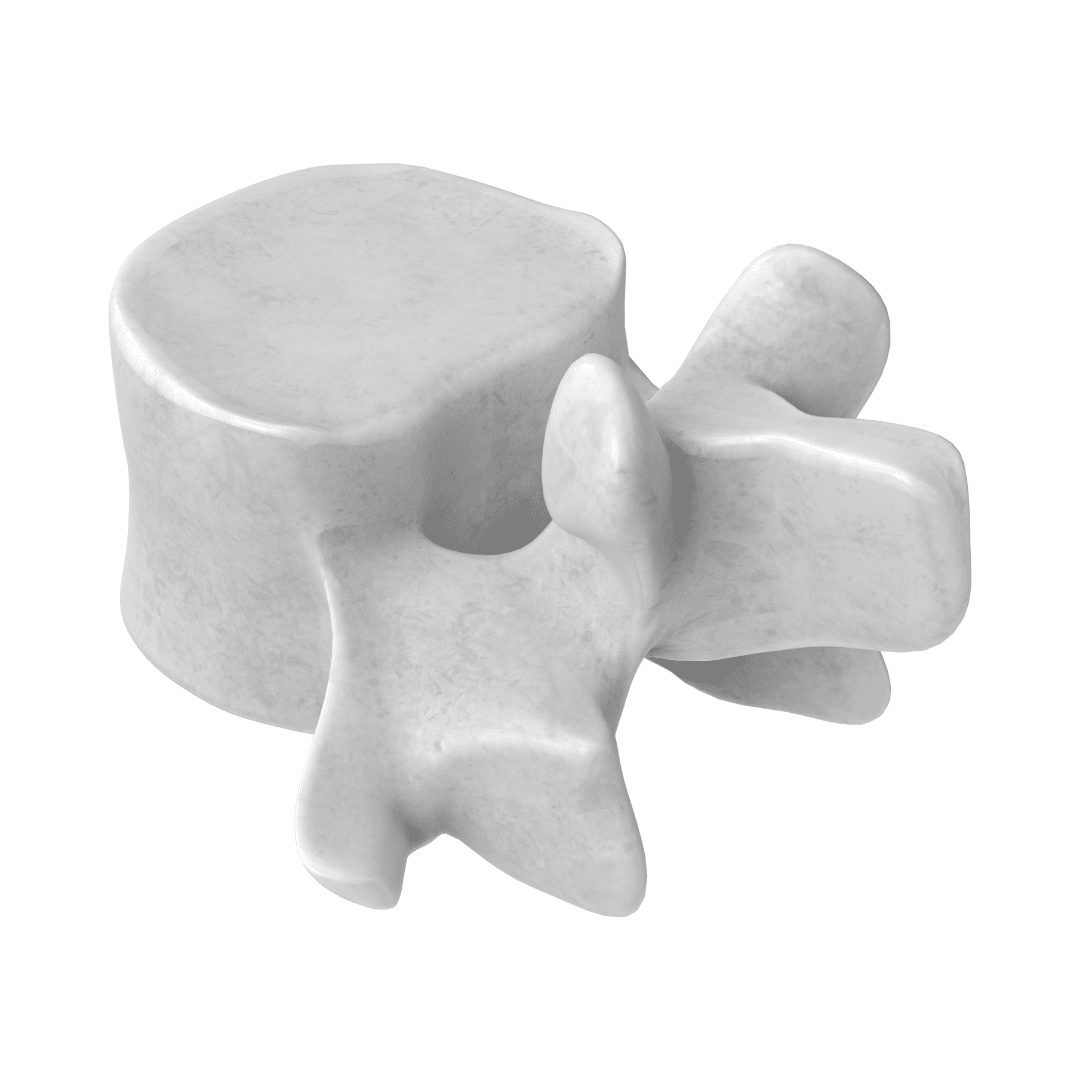
These facet joints are very important. They not only help guide motions at the lower back, but they also help prevent excessive movement between the vertebrae that might stress the important nerve and blood vessels traveling inside the boney ring. Due to them being the connection point between two vertebrae, you may hear injuries referred to in this way. You may hear about an L5/S1 stress fracture” which means that the bone of one level in this joint was over-stressed to the point that it developed a break.
These large nerves and blood vessels come from the heart and brain and split into smaller branches that supply the major organs, arms, and legs. Given their importance, they must be protected above everything else, and the different boney processes and facet joints do just this.
Also, these facet joints that serve as connection points between adjacent vertebrae are very important for common extension-based back pain in gymnasts. Injuries like face syndrome, stress reactions, and stress fractures (called spondylolysis & spondylolisthesis) directly relate to these structures.
Discs

Alternating with each of these vertebrae are structures known as discs. While these are not truly boney structures, they are directly connected to the vertebrae and serve as the main structural unit of the spine. These are circular structures that help to help the spine move, but also absorb and buffer forces of gravity.
These discs have an outer layer (called the annulus fibrosis) which is the outer ring-shaped wall of dense and resilient connective tissue. The fibers are obliquely angled to optimally handle high force gravity-based forces. it is important to note that the annulus fibrosis does have nerve endings, and can be a source of pain themselves.
The inner layer of these discs (called the nucleus pulpous), is made up of a gel-like, primarily water-based, ground substance. This viscous type disc material allows for enormous amounts of force absorption and movement flexibility that occurs during daily life and sports.
It is important to note that due to this outer wall and inner gel setup, each disc acts as a closed system. This means that it has a vacuum seal environment that allows for hydraulic pressure to be maintained. Due to this, the disc material on the inside of the disc displaces in the opposite to the movement of the lower back.
When someone rounds or flexes their back, the disc material moves backward. When someone arches or extends their back, the disc material moves forward. Compression forces from gravity cause the disc material to move outward in all directions in response to the downward pressure.
This concept is very important to keep in mind in relation to injuries like disc herniations and sciatica that will be covered below. The high compression forces, and the high forward bending repetitions from skills, are factors to remember.
Layer 2 – Ligaments
These bones and discs need support structures around them to not only maintain the spine’s position but also help limit extreme ranges of motion that might damage the underlying important tissues. This is where the various spinal ligaments come into play. Some of these ligaments are smaller, bridging one level of the spine to the next, to help prevent smaller micromovements. Others are broader, and more flat structures that travel the entire length of the spine and help to prevent larger movements. To help make people’s lives easier, here is a list of the most commonly referenced spinal ligaments, and the motion extremes they help to restrict. Again, all the research and textbooks for this information is below in the Refernences section.
- Anterior longitudinal ligament: extension
- Posterior longitudinal ligament: flexion
- Intertransverse ligament: lateral flexion
- Interspinous ligament: rotation and posterior shearing
- Superspinous ligament: excessive flexion
- Facet capsule/ligament: flexion and distraction
It is suspected that ligaments can be involved in lower back pain, particularly when very high sports forces place very high demands on certain areas of the lower back. Extreme ranges of motion, like excessive arching or rounding, are commonly seen in gymnastics and may irritate these ligaments.
Another important structure is the facet joint capsules. Remember that the downward articular processes of one vertebra connect with the upward articular processes of another vertebra to form the facet joints. Surrounding the connection of these two joints are facet joint capsules. They serve to add stability to the joint but more importantly provide nutrition and hydration in the form of synovial fluid. This is another structure that many researchers suspect can be a source of back pain, as they have direct innervation from the nerve roots of each level.
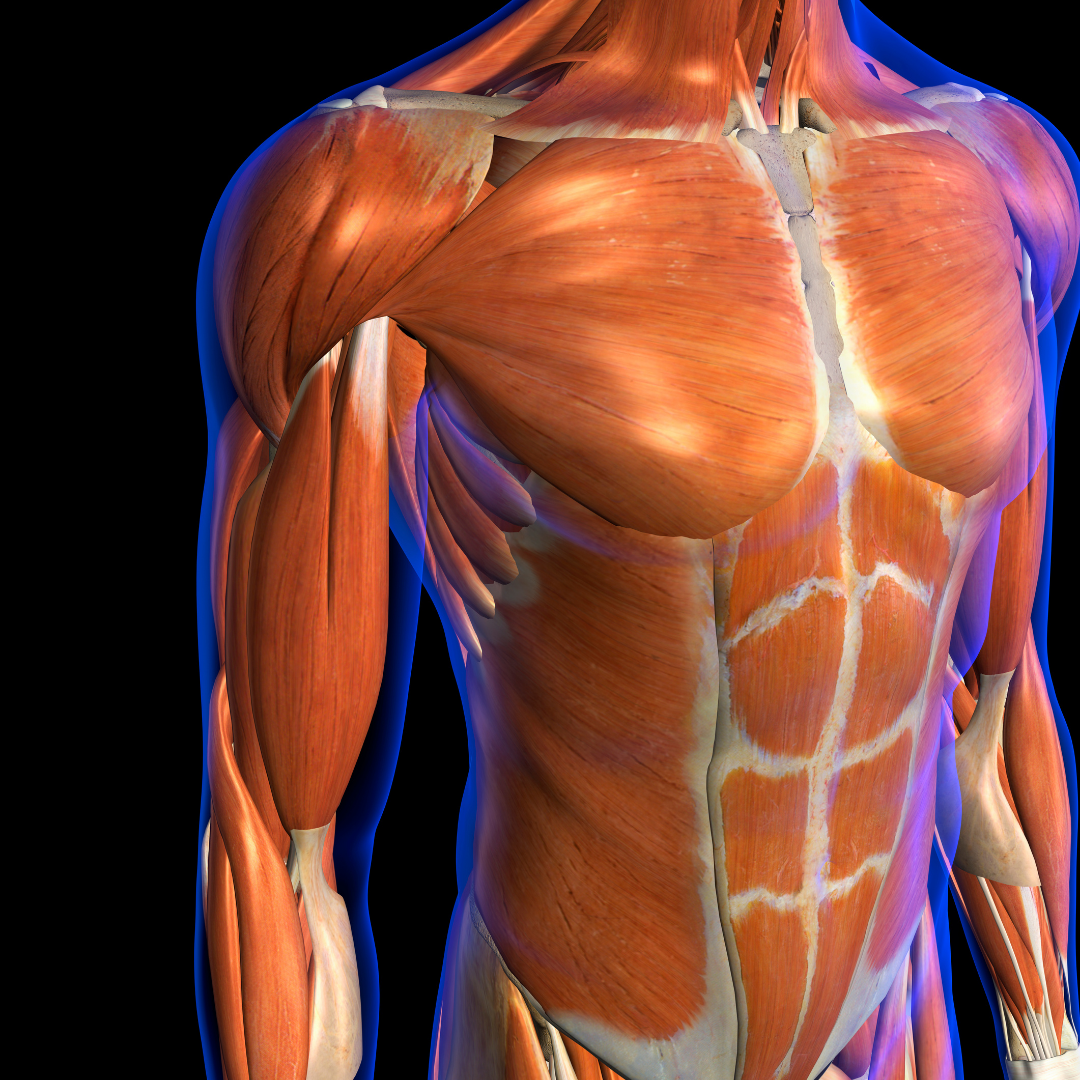
Layer 3 – Musculature
As has been described well by many researchers, the vertebrae, discs, and ligaments by themselves do not possess enough capacity to handle the average forces of daily life and the very high forces of sports like gymnastics. When taken by itself in cadaver models, the spine and the ligaments supporting it can not inherently take much loading before buckling occurs. That’s to say that someone is fragile, or should be fearful about “discs slipping” or “instability” as I will cover below. It’s more to note that due to the inherent static structural support, we need more dynamic support to help create, transfer, and absorb force. This is where the muscular comes into play.
Deep Musculature
Rotares, Intertransversari, & Multifidi
The deeper muscles of the spine, while less commonly discussed or known about, are incredibly important. Most of these different muscles tend to be smaller, span only a few vertebrae levels, and do not contribute to global movements of the spine like others do. The rotares and the intertransversari are two important muscles that fall in this category. They have a very small cross-sectional area, and play a much bigger role as “length transducers and position sensors” as researcher Stuard McGill puts it.
Another very important muscle that exists between individual spinal levels is the multifidi. Along with also having a huge role in joint position, due to it’s alignment running parallel to the compressive axis of the spine, it also works with other larger muscles to produce local extensor torque between segments. This is an important concept to keep in mind, as these smaller muscles are in place to prevent excessive translation between levels of the spine that may occur with very high forces seen in sports.
It’s important to note these much smaller, deeper muscles, tend to work reflexively and automatically in response to certain demands. Unlike larger muscles of the core, like the rectus abdominis or obliques, it’s a bit trickier to “flex your multifidi”. The training for these muscles comes through a variety of mechanisms including proper bracing and breathing patterns, as well as using different loading strategies to create stiffness.
Transverse Abdominis
There is no doubt that the transverse abdominis plays a crucial role in the core, and also must be included in the conversation about low back injuries. With that in mind, the wave of research in the 90s/2000’s claiming the TA was the “holy grail” of low back pain, and that everyone needed to be doing hollowing exercises, has definitely fallen out of fashion. Newer research (more here, here, and here) has supported that not only is the TA not directly linked to lower back pain, but hollowing exercises also don’t seem to “increase core stability” or reduce pain when compared to other exercise interventions.
That said, we certainly do need to understand the role the TA plays in overall core function, and not completely ignore it. The TA is a broad muscle that starts from the iliac crest, inguinal ligament, and thoracolumbar fascia and spans the entire abdominal space attaching to the lower rib margin. It’s very important for bracing and creating intra abdominal pressure.
This comes into play in many areas of gymnastics, particularly when we want athletes to be “stiff” and brace their core for skill work, but also when they are bounding and landing as seen in floor, vault, or various dismount situations. Also, it’s important that gymnasts understand proper bracing strategies when doing strength work, particularly weight training. With this in mind, many people ask what should be the focus to train the transverse abdominis if hollowing may not be the most effective strategy for sport carry over. This is where the diaphragm and pelvic floor come in.
Diaphragm & Pelvic Floor
As I will break down in the section below, the superficial core musculature can be thought of as a “canister” or “soup can” around the spine. The top of this canister is the diaphragm, which serves a dual role in respiration (gas exchange of oxygen in, carbon dioxide out) but also spinal support. It is a dome-shaped structure that has many attachment points across the ribs, lumbar spine, and sternum. At the bottom of this canister is the pelvic floor, which is a series of muscles that serves a dual role in maintaining organ alignment (particularly the bladder) and spinal support.
Based on some phenomenal research work by Leon Chaitow, we have learned that proper breathing patterns are one of the best ways to help foster reflexive activation of the deep core that serves both the breathing and the spinal support role the diaphragm/pelvic floor has. From its role in respiration, with proper breathing patterns the diaphragm contracts and flattens it helps expand the chest cavity and inflate the lungs. From its role in spinal support, the diaphragm helps to optimally align the “soup can” so that the force can be optimally dispersed during movement.
When someone is trained to use proper breathing and bracing strategies, the top of the core canister is perpendicular to the pelvis and pelvic floor. This allows the pressure to move from the top of the diaphragm, down to the pelvic floor, and then out into the surrounding superficial muscles like the obliques, to provide fantastic dynamic support of the spine.
Superficial Musculature
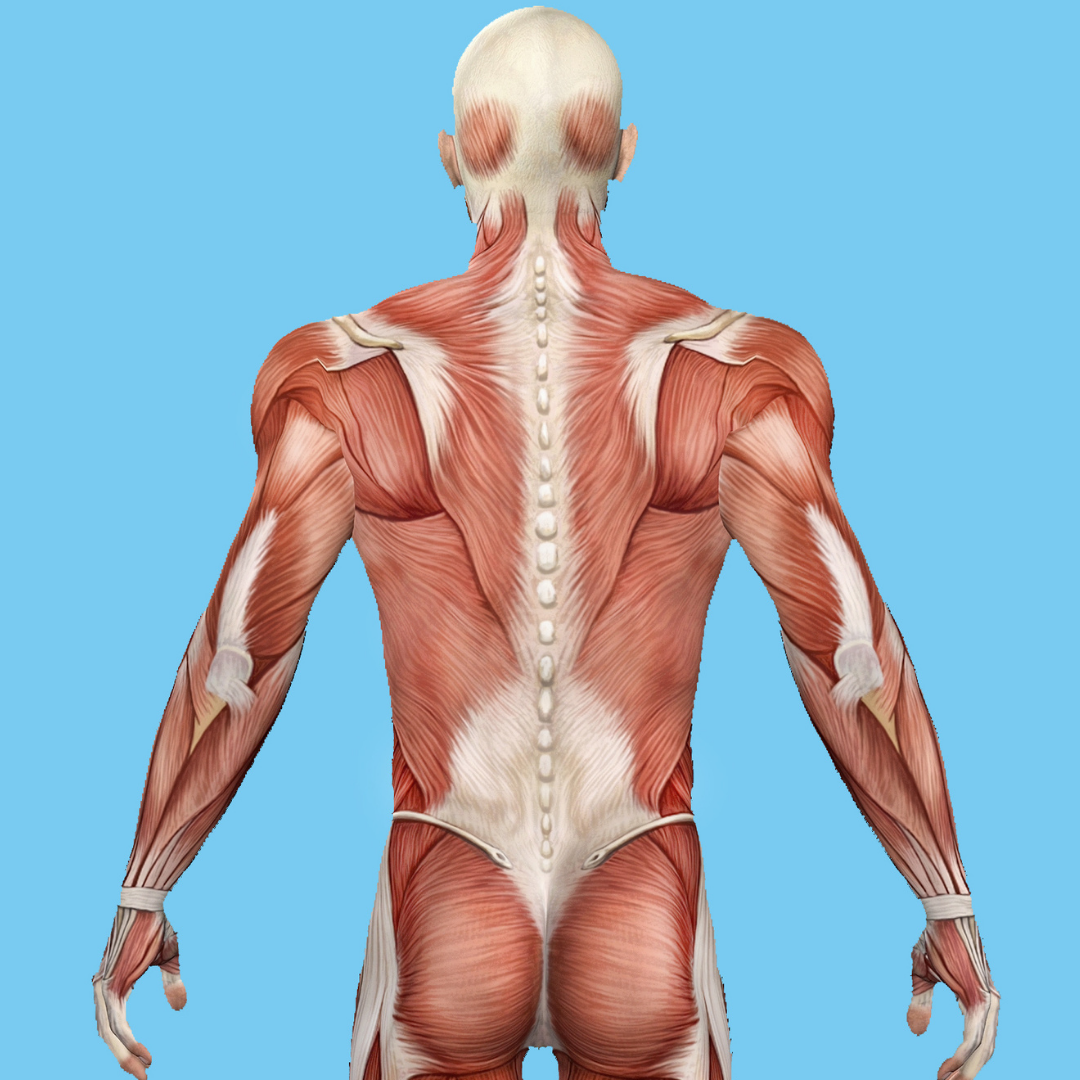
Moving on from here, it’s important to discuss the superficial muscles of the core. These are the more commonly known muscles that are larger, have more cross-sectional area, and are the main “show and go” muscles. They serve to create global movement at the spine while also transferring, buffering, and absorbing forces produced by the arms and legs.
Before breaking down specific muscles, it’s important to remember that all parts of the superficial core share an equal and important role. It is very common to see gymnasts training the front “6 pack” core and sometimes the obliques, while often times completely ignoring the other areas. If we neglect certain areas, or don’t train them all equally, it may create a situation where there is a “weak link in the chain” and we lose the overall core strength/capacity. As we create exercise and strength programs, this will be very important to remember.
It’s also very important to remember that the “core” is not just the abdominal muscles. It includes many larger muscles that span the entire length of the torso and pelvis. Muscles such as the latisimus dorsi, the iliopsoas,
Front Core – Rectus Abdominis

The rectus abdominis is located on the front of the core. It starts from the pelvis and inguinal area, travels up the entire front of the spine, and attaches to the lower rib borders and the sternum. It has bands of fascia that run through it, creating separations and the visually noticeable “6 pack” that people refer to. It works to not only flex the spine but also resist arching motions against gravity.
I intentionally put the rectus abdominis farther down the list of muscles to talk about, because in my opinion it is overly sensationalized by the mainstream media and some people. There is no doubt that we must train the rectus abdominis is important for gymnastics, particularly the compression and fast arch/hollow changing many skills and the ability to hold shapes tightly.
This said, just because someone has a “6 pack” or is very lean, does not mean that they have a strong core, can maintain great shapes, or brace their core properly against high forces. We do want to train this muscle, but equally, as much as the other areas to keep things balanced.
Back Core – Erector Spinae
In opposition to the rectus abdominis is the erector spinae. This group of muscles is actually a set of 3 small individual muscles. They are the Iliocostalis, the Longissimus, and the Spinalis. The Iliocostalis lumborum also sits near this group of 3 muscles. All of these muscles start from the pelvis and sacrum arae, span many joint/rib levels, and then attach at various points up the spine. They serve to resist backward shearing forces on the spine bones, but also can help to actively extend the lower back.
It’s very important to not only recognize these muscles but also intentionally train them to help build capacity against high gymnastics forces. In many gymnasts who may either not have strong glutes/upper back muscles, or who may just overuse their lower back naturally, these muscles may get overworked and sore. Also, if not trained they might not be able to handle the high impact forces that come with impacts and landings. This could create a situation where the lower back joints and bones become irritated.
Side Core – External and Internal Obliques

There are two oblique muscles on each side of the torso, one deeper layer of the internal obliques and one more towards the surfaces of the external obliques. These muscles are stacked on top of each other and are positioned in opposing 45-degree angles. They both start from the pelvis, and travel obliquely until they attach to the ribs and the rectus abdominal fascia.
The primary role of the obliques is to work with the transverse abdominis to flex the trunk when working together, or side bend / rotate the trunk when working by themselves on one side. However, they also have a crucial role in bracing the ‘soup canister’ given where they are positioned. The internal and external obliques are crucial to train, as they not only have a huge role in gymnastics performance but also work to protect the spine during high force skills.
Side Core – Quadratus Lumborum
Another important muscle that is positioned on the side of the trunk, and works with the obliques, is the quadratus lumborum. There is one of each of these muscles on each side of the trunk. The QL starts from the top of the pelvis, travels up the side of the trunk, and attaches to the higher lumbar vertebrae as well as the lower rib border.
The primary role of the quadratus lumborum on one side is to help work with the obliques and glute medius of the same side to prevent sideways tipping of the body when someone stands on one leg. The same one-sided QL can also side bend the trunk towards that side (left QL can contract to bend the trunk to the left). Lastly, another important role of both QLs is to extend the lower back. This is similar and in opposition to the obliques working together to flex the trunk.
The quadratus lumborum is important for a few reasons. One, due to how it works with the glutes and obliques, many people underlook training these muscles and find that balance/one-legged landings are challenging for gymnasts. Two, if the QL is undertrained it is very easy for soreness/pain to pop up with overuse or awkward landings. Three, due to how many gymnasts tend to have an over extended posture, training proper breathing/bracing mechanics can help to reduce the possibility of the QLs becoming over worked.
Latisimus Dorsi
While not directly a core muscle, due to its massive span and it’s starting point being directly on the lower back area, this is an important muscle to include. The Lat starts from the fascia of the middle and lower back (the thoracolumbar fascia) and has a huge base while it travels up and attaches to the inside of the arm bones. Because of this unique anatomy, the lat can be a very important assisted stabilizer of the core, and creating ‘tension’ in the lats during skill work can help further brace the core.
Along with this, the lats are one of the main power generators for skills on uneven bars, parallel bars, high bar, and rings. They also help forcefully close the shoulders for flipping and twisting. Due to this, it’s very common for the lats to get overly worked and stiff in gymnasts. Often times when this occurs, as the gymnast continues to try and use their arms overhead they may then lack the soft tissue flexibility for it and over-extend their lower back to make up the difference. This is an important thing to keep an eye on for overhead flexibility and skill performance (think archy handstands) but also for maintaining core position/bracing.
Iliopsoas
Similar to the lat, while the iliopsoas does not directly brace the core, it is massively important in this discussion. It’s not commonly known that on portion of the iliopsoas muscle actually starts from the vertebrae of the lower spine. It starts from these spine bones, travels down into the pelvis, blends with the other portion that starts inside the pelvis, and then becomes a tendon that attaches on the leg bone (lesser trochanter of femur).
Because of this unique anatomy, it not only can influence the degree of an arch a gymnast may have but also requires core bracing to have a firm base for the legs to create power from. As with the lat, this is an important muscle to not only maintain flexibility but also train in combination with the core to have the best overall performance.
Layer 4 – Low Back Nerves/Neural
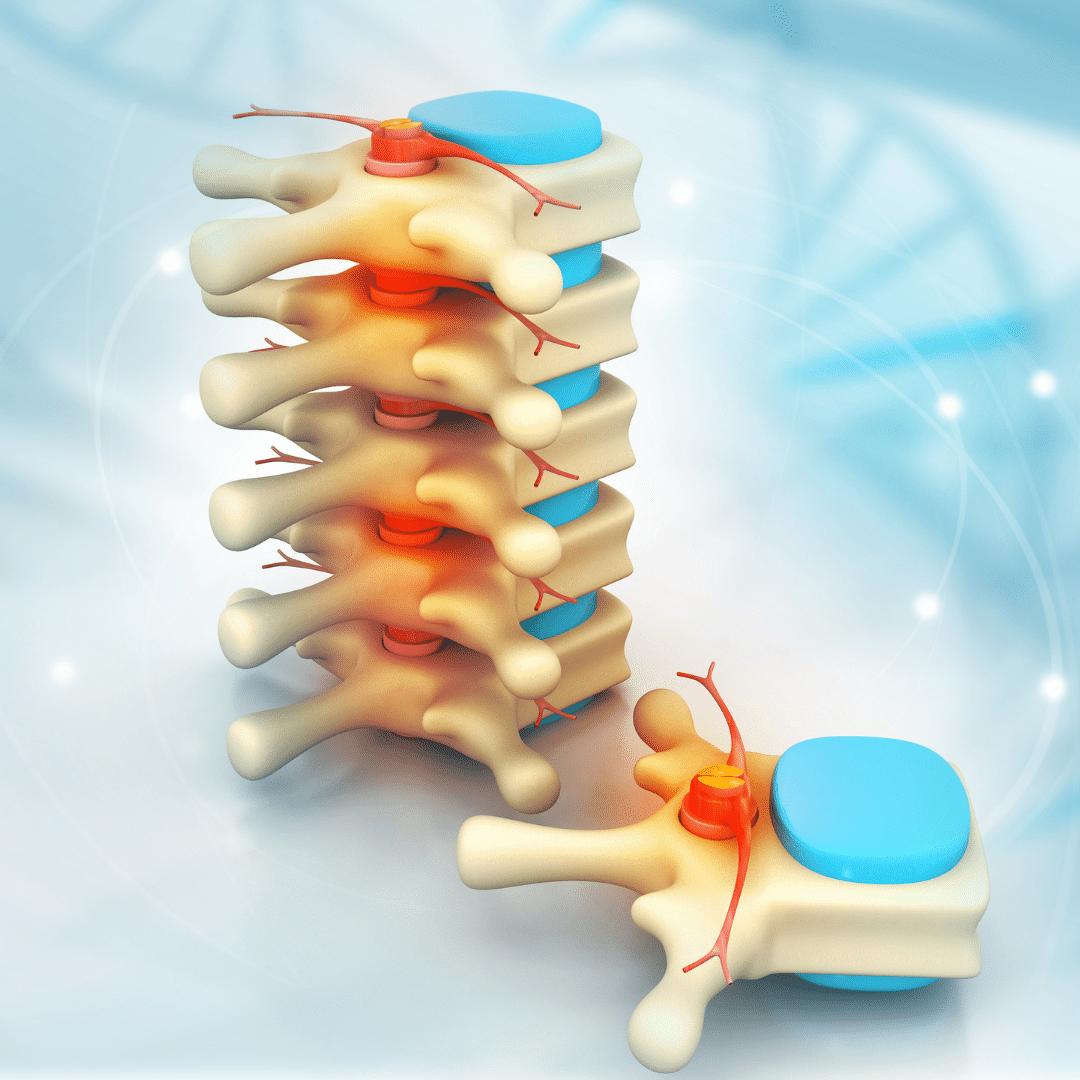
Once we move past the basic bones, ligaments, and muscles, we then can think about the nerves of the lower back. I often tell my patients that above all else, your brain cares most about protecting the spinal cord, blood vessels, organs, and ‘highway’ of smaller nerves/blood vessels that make that all happen. Due to this, there is a massive amount of boney and soft tissue protection built into the lower back to help the nerves and blood vessels stay as safe as possible.
As I touched on above, there is a ‘ring’ shape structure to each vertebra in the lower back with many smaller pieces extending off of it. This middle ring is where the spinal cord is housed, giving it tons of protection but also allowing signals to travel very fast up and down. Near this, protected by the other neighboring boney prominences, are the major blood vessels branches. This set up allows lots of smaller arteries and veins to maintain blood flow across the body.
Coming back to nerves, it’s very important to point out that between each set of stacked vertebrae is a nerve root that exits. You may have heard these referred to as “levels” and labels such as the “L5/S1 nerve root”. This is a way that medical providers help refer to specific connections between two vertebrae, and the corresponding nerve root that exits between them. Running down the entire length of the spine, there are nerve roots coming out from these different joint connection points. One on the left, and one on the right. This is why you may hear about the “left L5/S1 nerve root”.
While I don’t want to dive too much into the nerdy side of things, I just want people to know that these large nerve roots, and many smaller nerve branches, come from the levels of the lower spine. They are each responsible for information going in, and information going out, of the spinal cord from different areas of the pelvis and legs. As we will dive in more below, certain injuries might involve these nerves.
Layer 5 – Kinetic Chain
No conversation about the lower back and the core is complete without mentioning how important the entire connection of different areas of the body is. I want to briefly mention how some adjacent areas influence the lower back and common injuries.
Hips/Pelvis

You really can’t separate the lower back from the pelvis, to be honest. Whenever I treat a gymnast for lower back pain, I always evaluate and treat the hips and pelvis as well. This is because of a few things. One, the lower back position is directly influenced by the hip joints. Second, many of the muscles of the core and hips blend and interact with each other. Many core muscles have an attachment point to the pelvis, whereas many hip muscles have attachments and influences on the lower back/core.
If someone lacks flexibility in the front of the hips or the inner thighs, it can easily create a situation where the lower back has to arch more to make up the difference. Similarly, if someone really struggles with hamstring, pike, or compression flexibility, that can create a situation where their lower back takes more pressure during those skills requiring it. For these reasons and more, it is crucial that we always evaluate, treat, and keep an eye on the hips and pelvis when working on a lower back injury.
Thoracic Spine
In the same light, oftentimes if someone is lacking mobility in one area it might cause the lower back to overwork more during gymnastics skills. The most. This is most commonly seen in the upper back, known as the thoracic spine, followed by the hips and shoulders. If a gymnast lacks mobility in the upper back to extend and rotate, they may start to overuse their lower back more. This could create a situation where the structures mentioned above become overworked, or possibly the joints/bones of the lower back also start to become irritated. For this reason, we must always screen thoracic mobility and correct it, or teach a gymnast how to use their upper back/shoulders to take pressure off their lower back.
Shoulders

Connected directly to the thoracic spine is the shoulders. If a gymnast lacks the soft tissue flexibility in their latisimus dorsi, teres major, pec major, or pec minor, it might create a situation where they are unable to fully open their shoulders past their ears during skills. One of the most common compensations we see for this is the lower back arching more to make up for it. There are many gymnasts who I have treated for back pain that was not getting better, and one of the reasons for this was that no one ever screened and corrected their shoulder or thoracic spine mobility.
On the same line of thinking, there are times when it is not so much a limitation in mobility but more so a limitation in strength or active use of that available flexibility during skills. Sometimes, gymnasts have all the mobility in the world but do not apply it during skills or may not have enough strength in those areas to handle high forces. This is where great strength programs, great progressions, and great technique come into play.
Ankles
Lastly, one less common but important area to mention is the ankle joints. Due to all of the heavy landings and toe pointing that gymnastics required, often times gymnasts will lose their ankle mobility in the “toes up” or dorsiflexion motion. This can create a situation where when gymnasts lands, they are unable to use the proper squat-based movement pattern. One of the possible compensations that may occur, is that a gymnast may over round or over arch their lower back. While this is not always a clear sign of injury risk, it is something that my overtime create lower back irritation. Similar to the reasons above, I always try to look at ankle mobility in gymnasts that I treat for lower back pain.
What Are The Most Common Lower Back Injuries in Gymnastics?
Movement Categories of Back Pain in Gymnast
Without going way down the rabbit hole of nerdy lower back research, I will start by saying that I tend to evaluate and diagnose gymnasts for back pain based on movement categories. There is obviously way more to the process that is elaborate, but my aim with this blog post is to make it accessible for the majority of people. So we will only focus on this concept of movement categories, and understanding how different skills may create common injuries seen.
There are 5 main movement categories of lower back pain that most gymnasts deal with. They are ordered from most common, to least common.
- Backward Bending or Arching (Extension)
- Can also be with rotation, if on one side of the back
- Forward Bending or Rounding (Flexion)
- Can also be with rotation, if on one side of the bac
- Impact or Compression
- Can also be with flexing, or extending, based on the skills
- Hanging or Traction
- Rotating or Twisting (Sidegliding used as a proxy)
With these in mind, we will break them each down and talk about the common injuries that can be seen in each category, in order of most to least common.
Backward Bending or Arching (Extension)

The first, and most common, the category that gymnasts have pain with is backward bending or extension. This is typically pain felt with any arching skill like back/front walkovers, front/back, handsprings, arching tap swings, Yurchenko’s, extreme jumps and leaps, and so on. Gymnasts may also feel soreness with standing upright, lying on their stomach, leaning backward, or having a heavy book bag on their shoulders during the day.
Remember that on the backside of the lumbar vertebrae, we have structures that extend to form the facet joints which connect one vertebrae to the next below it. When a gymnast bends backward, or arches, to extreme ranges of motion, these facet joints close completely. Depending on whether this happens many times over the course of weeks/months, or if one high force dynamic skill extends their back forcefully at one time, injuries to these structures may occur. They tend to happen on a continuum, moving from less time of irritation/severity to more time of irritation/severity. If a gymnast has pain with these types of back bending skills, but does not speak up about it or does not stop doing things when it hurts, things may rapidly progress to get more intense.
I tend to use a standing back bend, Stork test, prone press up, prone on elbows extension and rotation, and PA shearing test to look into this category.
Facet Syndrome
On the far left side of the time/severity continuum, is what is known as Facet Syndrome. This typically refers to irritation of the facet joints themselves, and the structures around the facet joint. If a gymnast does these extension-based skills over and over, or possibly has one skill that for some reason puts more pressure on the facet joint, it may create local tissue irritation of the muscles/ligaments/joints, and a pain output by the brain to help limit movement. There may actually be some local inflammation of the tissues as well.
It is always hard to know exactly what structure is referring to pain in a gymnast with this type of pain. This is why I tend to evaluate and treat people based on movement categories. It may be the actual joint, or the joint capsule, or the muscles around the joint, or the nerve endings close to the joint, that are referring pain.
That said, gymnasts often will feel diffuse stiffness or aching pain in their lower back to start. They also might feel ‘spasms’ in their lower back, as the body tries to help splint and further protect the joint that is irritated. This can occur on one side of the back (called unilateral) or on both sides of the back (called bilateral).
Typically, a gymnast will be aware of their lower back pain but due to their stoic/stubborn nature may not speak up about it. They also might be a little embarrassed about it, and not mention it to their coaches and parents thinking “it’s fine, it’s just part of gymnastics.” or in fear that some coaches will dismiss their complaints. They may also have an important competition they want to compete in. For whatever reason, in my experience most gymnasts typically tend to keep training through this pain unti it gets worse, which is where stress reactions come in.
Stress Reaction
The next step in the time/severity continuum is a stress reaction. In this situation, not only are the joints themselves irritated, the actual bone that connects the facet joint to the vertebrae starts to get irritated. Remember that the “downward” facing articular processes of one spine level connect to the “upward” facing articular processes of the spine level below to create these facet joints. When a gymnast backbends repetitively, and the facet joint is completely locked out, the stress then shifts to the ring of the vertebrae (vetebral arch or neural arch).
This specific structure that takes the stress is called the pars interarticularis. This is a portion of the vertebral arch that connects directly with the body of the vertebrae holding the disc. The back bending motion of many gymnastics skills pushes the pressure through the facet joint, down the articular process, and into the pars interarticularis in a forward direction. This pressure on the pars over time with more high force repetitions causes tiny micro damages in the bone. Just like above, this can occur on one side (unilateral) or both sides (bilateral) of the lower back.
If repeated over more days, weeks, and months, it can cause the bone to start micro fracturing slightly. This “start” of a fracture is referred to as a stress reaction. It means that while the bone is not fully fractured all the way through, the start of one is there. If a gymnast gets a highly sensitive MRI, a bone scan, or a CT scan, this can often be seen. This is definitely more severe than more basic facet syndrome or muscular irritation issues.
Gymnasts in this category are typically in much more pain, and are much more limited in both their daily life and training. Standing for extended periods of time is much more uncomfortable, they have a tough time doing back bending skills, landings might start to become painful, and even just running might cause them pain. Along with this, gymnasts might also start to have pain with forward-based motions like bending over or hollowing motions if the lower back muscles are also irritated and trying to splint/spasm to protect the bone.
Spondylolysis (Stress Fracture)
Unfortunately, even though gymnasts may be in notable pain and they might notice something is not going well, they may continue to train for a variety of reasons. Sometimes, it’s not malicious intent .It’s just the sport being very hard on a young, growing body of a child. Even the most amazing parents/coaches don’t realize that this is occurring and continue to train.
This can lead to a situation where the pars interarticularis does fully fracture through, which is called a Spondylolysis or stress fracture. This type of fracture is referred to as a “fatigue” fracture because it takes hundreds and hundreds of repetitions of back bending over many weeks/months to cause the bone to finally “fatigue” out and break. These breaks, again, can occur on one side or both sides of the lower back.
This is a very challenging, and upsetting, situation for many gymnasts and their parents/coaches. For one, when the bone actually breaks it is typically very painful and limiting. It can have a huge negative impact on the gymnast’s quality of life. This is both from a physical health and mental health perspective. Second, it also takes a notable amount of time to recover from. It takes about 3 months for the bone to heal (on average), and then another 3 months to go through formal Physical Therapy, and then another 1-2 months to rebuild back up to their pre-injury skill/routine level.
For this reason, it’s absolutely crucial that very honest and open communication is used when a gymnast’s back starts to hurt. It is also why preventative measures are needed way before someone’s back may start to bother them (more at the end of this article).
Spondylolisthesis (Stress Fracture with Vertebrae Movement)
On the very far end of the time/severity continuum, is when the vertebrae that have had the fracture in it starts to slide forward in relation to the vertebrae below it. This is referred to as Spondylolethesis, and only tends to occur when someone has fractures on both sides of their back (bilateral). This happens because there is no longer a boney anchoring point of the vertebral body, and with continued arching motions the body can slide forward.
These injuries are graded based on the percentage of movement that is seen on imaging compared to the vertebrae below. Grade I refers to 0-25% motion, Grade II refers to 25%-50% motion, Grade III refers to 50%-75% motion, and Grade IV refers to 75% or greater motion.
These injuries are, unfortunately, much more severe and must be taken very seriously. The main reason is that the sliding motion of one vertebral body starts to put pressure on the large nerve roots, and possibly the spinal cord, as well as the major blood vessels around the spine. While nerve or traveling radicular pain is typically associated with forwarding bending (more below) progressions of spondy fractures can also lead to concerning nerve issues. If someone starts to experience traveling pain, numbness in their legs, or other red flags, they must consult with a spinal specialist ASAP.
Spinous Process Impingement
Spinous process impingement is a separate category of injury for backward bending-based pain. While the same types of motions tend to create this injury, it involves the spinous process which extends backward off the middle of the spine, and not the facet joints/pars that is on one side of each area of the spine.
If a gymnast has a very hyper-flexible spine or unique anatomy, they may be able to back bend very far without causing too much irritation to the facet joints. They instead might cause the two neighboring spinous processes to hit each other, and create bruising over time. I tend to see this more in rhythmic gymnasts due to the extreme motions and esthetics skill goals they have. Pain is typically felt directly in the middle of the spine, and palpating the spinous processes themselves may reproduce their pain. Also, imaging may show inflammation of the spinous process instead of the facet joints or pars interarticularis.
Forward Bending or Rounding (Flexion)

In complete opposition to backward-based extension pain, is forward-based flexion pain. Remember that when looking at the anatomy of the spine, we do not have joints on the front of the spine that prevents excessive forward bending from occurring. We do have some ligament structures, and muscles, to prevent extreme motions. But, it is not quite the same ‘hard’ top to back bending that the facet joints create. With this in mind, let’s chat about some common injuries in the forward or rounding-based category with the same time/severity continuum in mind. I tend to use a toe touch, quadruped rock back, seated compression test, and slump/straight leg test to look into this category.
Muscular Spasms
The most common, and often least severe, types of lower back injuries in gymnasts are simple muscular irritations or spasms. These tend to happen all the time as the sport is just demanding, risky, and comes with many awkward movements/off landings. In this situation, usually a gymnasts back is over worked in a short period of time, or maybe they just fall awkwardly doing a skill, or maybe there are other factors outside of training that make recovery tough.
For whatever reason, these small spasms tend to be uncomfortable, but not the worst thing ever. Gymnasts will usually have stiffness and soreness if they bend forward, sit for a long time in school/in a car/on a couch, or bend over a lot doing homework and studying. They also might not feel great with flipping skills, kips, or certain hollow-based conditioning. In my experience, they usually have limited training and soreness for 1-5 days, but things generally calm down if they rest and take care of themselves properly.
Discgogenic Pain
Moving on from the simple spasms, comes a bit more long duration, and a more intense type of irritation. Remember that in the lower back, the disc material moves opposite to the motion that someone does. So if a gymnast rapidly flexes their spine under high load (think in bars, flipping skills, or hard landings) many times in a row, it might start to create some sensitivity of the muscles, disc wall, ligaments, and joint capsules.
It’s important to remember that the outer wall of the disc, the annular wall, can in fact refer to pain. Beyond that, a common situation that may occur is with lots of high force, dynamic flexion of the spine may cause the disc material to move backward and create a building. It’s crucial to note here that a disc bulge is not inherently dangerous, or bad, or will automatically cause pain. Plenty of people have disc herniations with no pain, and some people have minimal disc building but notable pain.
This said, sometimes disc bulges may create pain levels either through the annual wall getting stressed, or possibly pressuring being put on the nerves right next door to the annular wall. This not only may create local pain inside the lower back, but in some cases can create nerve irritation that sometimes causes traveling pain.
Now I will be the first to tell you, there is a huge debate in the Pain Science vs Mechanical medical world on what really is going on here in relation to what is causing pain. The more pain science approach would be that there is some sort of perceived threat on the tissues, that the brain is outputting pain to protect the person from moving further into that sensitized motion, and that reducing threat via workload modification and exercise is the way to help.
The Mechanical world approach would be that the forces of gymnastics/life have actually created small amounts of local tissue damage and inflammation, that the chemical irritation is creating localized sensitivity and the brain’s pain output to protect further irritation of those sensitive/damaged structures, and that reducing load via workload modification and exercise is the way to help.
Regardless of the ‘camp’ that you hitch your wagon to, at the end of the day it boils down to rounding of the lower back, and high load dynamic flexion in gymnastics skills creates pain. Due to this, we are going to want to approach that with caution to unload the back to lots of hollow-type forces and help move the athlete into extension-based motions to take pressure off the disc/nerves.
Sciatic/Radicular Pain
The last full progression down the rounding or flexion-based continuum for pain/severity is when the disc bulging or nerve irritation continues to develop. In this situation, this can cause a significant amount of back pain as well as leg pain and lost functional ability. Whether it is the disc bulge putting pressure on the nerve root, the nerve root itself being irritated for a non-disc related reason, or high peripheral sensitivity coming from another mechanism, these conditions are very limiting.
Often times gymnasts will have very stiff, rigid posture in fear of flexing their due to acute muscle spasms, local back pain, and traveling leg pain. Simple activities like putting on shoes, leaning over a sink to brush their teeth, sitting in a car or chair for school, and many other basic things become painful. Oftentimes, attempting any gymnastics is out of the question due to how much pain is going on.
If you look at the literature, typically these types of disc herniations over time can get better with rest, proper exercise, and activity modification. As I mentioned, the degree of disc bulge doesn’t always correlate to the degree of pain. Also, some studies show that disc herniations naturally absorb back into the central disc space over time. There are other studies showing that proper exercise and treatment progressions can help significantly to reduce the bulge. There is also great pain science education research that just teaching someone about their back pain, helps them understand why they are in pain, and gives them some simple strategies to understand that their discs aren’t “slipped” or their back isn’t “a mess” can help reduce sensitivity levels.
That said, there are some situations that can get someone into hot water very fast. Remember that the disc is enclosed by the outer annular wall and that this closure allows for hydraulic pressure and a ‘vacuum’ type environment to be created. If the disc bulge happens to get worse over time, or if something very traumatic happens that causes the disc material to move outside the annular wall, this could be a much more serious situation. Because the “closed” system element has been lost, exercise progressions to help relocate the disc material might not be as effective. Also, those exercise progressions might actually cause the disc material to press on the nerve root, causing significant amounts of pain.
If a gymnast has notable nerve pain, or traveling pain, it really is best to get them seen by a doctor who is a spinal specialist. Any “red flags” like numbness or tingling in the groin area, a loss of muscular strength in the legs/feet, sudden weight loss, or pain that is constant through the night, all warrant immediate investigation.
Impact or Compression

The next major movement category that can trigger pain in a gymnast is impact, or compression. I intentionally wanted to put compression a little bit lower down on the list, as in my experience the majority of problems with impact are also tied to either extending or flexing of the spine. Based on the type of skills that create pain, and the story that a gymnast tells me, I will go down the path of teasing out if impact is the driver of their pain. I tend to use jumping and landing, a heel drop test, and a seated compression test to look into this.
Impact + Extension
I oftentimes see that gymnasts doing punching skills without the best core position, core bracing, or technique, have this issue. Younger gymnasts who maybe have not quite developed their technique yet, or someone who may not have the strength to combat the high forces of gymnastics, are in this category. Some of the more basic skills like punch fronts on the floor, or even just hitting the springboard, can be problematic if someone hits in a very large arched back posture. I also see this very commonly in optional gymnasts who are doing connection passes, like one and a half to a punch front pike or layout.
Remember that the facet joints are more ‘closed’ when someone is arching or in this extended posture. If they do not have the core control or core strength to know how to maintain a good spine posture, the forces of impact may cause the facet joints to rapidly close, and compress. This could create local muscular pain, but also possibly irritation from the joints themselves. This is also important to keep in mind as sometimes a gymnast with a stress reaction or stress fracture might get pain with both arching backward and arching impact.
Impact + Flexion
In a similar light, there are times when gymnastics landings or dismounts put a gymnast in a very rounded, flexed spine posture. The highest recorded force on the spine in gymnastics during maximal flexion is 40x bodyweight. That is an astronomical amount of force. When the spine compresses under a high load of an impact like this, the disc material moves outward in all directions to help buffer this. If a gymnast were to land in a very rounded, or flexed spine posture, the disc material will move backward more relatively.
Just as with the discogenic pain section above, this can not only cause notable stress on the muscles, ligaments, and joints of the spine but also possibly cause the disc material to press against the nerve root. If a gymnast takes one bad landing, it oftentimes is more muscular in nature. If a gymnast lands over and over in a not great position, that is when things start to progress to more intense back pain or nerve-related issues.
Impact Alone
Although less common, there are times when simply the impact itself is the trigger for pain. Someone could land in what looks like an idea, neutral core position, but still have pain. On top of each vertebra is something called an endplate. It anchors the disc to the bone, but also helps to add additional buffering support through cartilage layers. There is also a growth plate located on the back of each spine bone.
Sometimes in young gymnasts who are not fully matured yet, the high force impacts of gymnastics can start to irritate the end plate or the growth plate. This might be one cause for back pain with landings. The other might be that the smaller muscles between the spine joints (multifidi, rotares, etc) could be getting irritated during these high-impact landings. By watching video, and using the clinical tests mentioned, we can get a good idea about if this is a causative factor by itself.
Hanging or Traction
Similar to impact, I find it rare that just hanging alone bothers a gymnast’s back. It is almost always in combination with arching or hollowing during skills. I see this most commonly in male gymnasts who are doing very high force ring giants, high bar taps for releases/dismounts, or are doing parallel bar tapping skills like Moys/Tipelts/Bhavsars. In female gymnasts, it can also happen with higher intensity release or dismount taps on uneven bars. But, due to the uneven bar rails being more forgiving on tapping forces, it doesn’t seem to be as common as male gymnasts.
While it is not fully known, the theory with traction-based back pain is that tissues known as the “Sharpey’s fibers” might be the source of pain. These fibers anchor the disc to the endplate/growth plate. With extreme traction forces, it is possible that these fibers are experiencing lots of shearing or pulling stress. It could also be the case that the muscles and ligaments of the spine are going through very high traction forces that they are not accustomed to. Doing a prone traction test with extension can help to sort this out.
Rotating or Twisting
I included rotating or twisting as the last category, but being completely honest I almost never see this as the main cause of someone’s back pain. It is almost always in conjunction with extension/arching (like punching into beam dismounts of floor back twisting) or flexion/hollowing (landing off to one side). There are very rare situations where someone can have a lateral disc bulge, in which side gliding assessments can be used to rule it in along with an MRI. Due to how rare it is, I would encourage people to go through all of the screening and other processes noted above first. If nothing shakes out as positive, then you can go down this path.
For a good summary on everything covered in this section, here is a popular video I made on SHIFTs YouTube Channel
How Long Do Low Back Injuries Take To Heal?
Respecting The Body’s Healing Process
The question that I get from gymnasts most when treating them for back pain is – “when can I go back to gymnastics?” or “can I compete?”. I completely understand athletes wanting to get back to training as fast as possible. It was the same for me as an athlete, and the coaching side of me certainly knows the challenge of having an athlete at practice hung up by these injuries yet wanting to make progress.
That said, we can not magically speed up basic human biology. There are certain things we can do to accelerate, assist, and enhance the natural healing process. But at the end of the day, we have to understand and respect the body’s healing timelines. There is a base timeline for various tissues of the body, and when looking at the literature a realistic timeline for various degrees of injuries. Unfortunately, these don’t change even if we are in the middle of competition season or ahead of a very exciting opportunity.
In almost all cases, taking the time to allow full healing and rehabilitation is the better choice. I’ve been fortunate to work with a few of the world’s best elite and Olympic-level gymnasts/coaches, and I can tell you that the situations where someone has to ‘push through’ for their ultimate goal are few and far between. They occur, but very very rarely. Not to mention, these decisions are often made by adults, their parents, and their medical providers as a team. With this in mind, let’s review some timelines for these various injuries.
Timeframes and Variability for Back Injuries
We must keep in mind that while there is great science on the healing timelines for many common back injuries, there is still a huge variability that can occur. In the big picture, factors like age, genetics, skill level, genetics, past injury history, and more all play a role. Also, the severity and reoccurrence of the injury will make a huge difference in the overall healing timeline. Also, as you can see above, there is a huge spread in the different types of movements that cause pain, the skills that re involved, and what structures might be irritated.
Oftentimes I will hear people compare one gymnast’s injury to another. Saying that “X” back injury took 4 weeks in one person, so a sort of similar “Y” injury in another person will be the same. I strongly recommend people do not do this. Even with what seems like the exact same injury, say stress reaction or muscle spasm, due to many factors mentioned above and more the full return to gymnastics this could be wildly different.
A stress reaction in a 12 year old Level 7 female gymnast who can change their beam series to a cartwheel round off, and switch to a Tsuk instead of a Yurchenko, might have a much easier time of healing and get back to gymnastics compared to 15 year old Level 10 female gymnast who has to do a layout step-out series and Yurchenko. Not to mention one stress reaction may be completely different from another in terms of the structures involved, outside gym factors, and inherent anatomy differences between athletes.
My best advice is to follow the science of healing timelines (and physician/surgeons protocols when appropriate) but use the major milestones of healing as a guide. These include education, mitigation of pain, restoration of mobility, a return to daily activities, return of full strength/power, and the ability to tolerate all advanced plyometric skills. I also always teach people early in the rehab process that during the middle of a rehab, when their pain may be gone, they will want to go back to sports but we have to resist the urge. Building strength, power, and capacity take multiple months and lots of work.
A useful rule of thumb to use with people is that for however long a gymnast is out of practice with their injury, it will take 2-3 times as long to return. So say someone has a mild muscle strain that keeps them out for 2 weeks, it will likely take them 4-6 weeks more to fully return. If someone has a stress fracture that keeps them out for 3 months, it will likely take an additional 3-4 months to get back fully.
This being said, in my experience and based on the scientific literature, with less severe injuries like muscular strains and low level joint irritation, it could be very benign and only take 2-4 weeks to recover.
As the severity of the injury progresses, the timelines extend. Higher degree muscular strains, disc or nerve issues, or stress reactions, the timeline may extend into the 4-8 week range.
Lastly, the most severe injuries occur like full spondy fractures, sciatica or significant nerve pain, end plate fractures, and decompression surgeries may easily take 4-6+ months to recover from.
The 4 Phases of Rehabilitation & Goal Milestones For Recovery
When I lecture, do consulting work, or provide rehabilitation for gymnasts, I always try to outline these 4 phases general of rehabilitation. Regardless of the injury, all athletes progress through them. Some injuries move fast if they are less severe, and some move much slower if they are more severe.
However, in general, I will say from the start that lower back pain tends to be a bit more challenging to deal with and overcome, as compared to maybe an ankle sprain or a forearm issue. For one, it’s hard to “not use” your back and core. Every day when you walk, move, and do things, the lower back is involved. This is unlike an ankle, which you can use crutches and put in a boot. Second, remember that the large nerve roots and important blood vessels are in the spine. Your brain cares most about protecting them, so it may output pain for longer or more intensely to help protect them at all costs. Lastly, gymnastics is extremely demanding on the lower back. Even the most basic shapes, conditioning, and technical work can be hard on someones lower back who is recovering from a bout of pain.
Also, for me recovery refers to fully getting back to gymnastics without physical or mental hesitancy. Being ‘cleared’ by a medical doctor from a tissue healing point of view doesn’t necessarily mean being fully ready to return to full gymnastics practice. I know and work with many amazing gymnastics-based medical providers, but I know not everyone has this luxury. This is why I try to abide by the 4 Phases of Rehabilitation. They are as follows,
1. The Acute/Subacute Phase – “Put The Fire Out”
This first initial phase is all about trying to understand why someone is in pain and reduce their symptoms while also helping educate them about what’s going on. This is generally in the first 4-6 weeks. We have to make sure that we really follow a good evaluation process by talking to someone, and also going through an in-depth movement assessment. I spend a long time when I first meet someone listening to their story and figuring out which category about back pain they fall into. From there, once we have. a good working theory I aim to do the following to help them get out of very high levels of sensitivity and pain.
Reduce Low Back Workloads
This is what no gymnast, coach, or parent wants to hear, but it’s a reality. The truth is, if someone is going through quite a bit of back pain and they are at the point where they are seeing a medical provider, there will likely be no “magic exercise” or “perfect stretch” to get their problem to go away. These types of injuries tend to slowly progress over time, so they will take time to calm down. Our brain oftentimes turns up the sensitivity levels to movements in an effort to protect us. So, we want to first talk about the need to think in “weeks and months” not “minutes and days.” Gymnasts will need to take a break from skills or routines, even if in the middle of season sometimes.
Maintain Global Activity Level
This said the research is clear that complete rest might not be ideal for back pain. We want to encourage a gymnast to do what they can to maintain activity levels. For some that might be no gymnastics at all, but going for walks and basic exercises from PT. For others, that might be no actual event work but still doing strength, physical preparation, and basic flexibility work. It is hard to know for sure, as each case is different, but if possible we want to reduce the exposure to skills that cause pain while trying to maintain as much activity as we can. A skilled medical provider can work with a coach and a gymnast to create this.
Educate on Directional Preferences and Daily Life Modifications
One of the biggest reasons we need to know what is movement category is causing pain, is so that we can help use the opposite motions to make someone feel better. If a gymnast has a lot of pain triggered by back bending or extension, we are going to want to educate them on how to do the opposite. I tell gymnasts who have pain with arching that they can do some hands and knees cat camels that only move from neutral to hollow, and rock back deep breathing drills, throughout the day to help reduce acute pain levels. I also tell them how very long periods of standing or walking might be problematic in the first few weeks, so building in times to sit can help.
In the opposite light, I tell gymnasts who have pain with rounding or hollowing to use cat camels moving from neutral to arching, and time laying on their stomach, to help. Doing small press up exercises, or mini backbends throughout the day, can be very helpful. I also tell them to not sit in low couches, and if they do sit try to put a rolled up sweater in the arch of their lower back ot prevent excessive rounding. I also tell them to set a timer and try to not sit for more than 20 minutes in the first few days.
As you can see here, it’s crucial that we know why someone has pain so that we can help them do the opposite. It may not be an instant fix, as sometimes the first 7-14 days can acute pain that is more chemical inflammation in nature, or acute guarding, that doesn’t respond super well to any motion. In this case, I tell gymnasts to do whatever they can to be comfortable, maintain a regular routine of switching positions, and to start PT ASAP for pain relief strategies.
Maintain Local Core Activity Levels

There is really interesting research from Paul Hodges and others that when someone has an acute bout of pain output, the activity levels of muscles within the lower back and core change. It has been shown that not only does muscle activity within a muscle change to adapt and help reduce the load on certain areas, activity between muscles in the lower back and core also change. This is thought to be a short-term, adaptive strategy to help reduce the load on sensitized structures. This is why you may see someone walking very stiff or rigid, or have a limited ability to move in all directions.
With this in mind, I believe that trying to maintain as much activity levels (while in a safe context) is crucial. As long as someone is not having an increase in symptoms during or in the few days following PT, I will try to give them neutral basic core exercises. I don’t think we are getting someone stronger necessarily, but more keeping them active and trying to maintain load in the core/lower back. In the pain science literature, it is thought that maybe this helps to reduce the acute sensitivity levels over time along with proper education strategies.
I tend to give people 90-90 breathing and core bracing drills first to learn about the basics. Then, I try to get them to bird dogs, dead bugs, bent knee side planks, bent knee front planks, and 1/2 kneeling anti-rotation press outs. I find that these tend to be tolerated better as they are in a move relatively neutral position, and lower threshold.
Address Issues Above or Below The Lower Back
One of the most common things I see missed in gymnastics low back pain rehabilitation is looking at the whole body. As we broke down above, the shoulders, thoracic spine, hips, and ankles play a huge role in back pain. While a gymnast might have pain at their lower back, the issue could truly be above or below that is causing their back pain. Just treating someones back pain, but not looking at their entire body or their training program, is like trying to put out a fire by simply pulling the smoke alarm batteries out. While it may make the alarm turn off, it hasn’t actually fixed the issue.
If a gymnast really struggles with shoulder/thoracic spine mobility, or maybe isn’t as strong as they need to, or maybe doesn’t have the best technique during skills, that must be addressed. I always spend a significant amount of time breaking down the shoulders, upper back, hips, and ankles for mobility or strength issues. I also talk a lot with them about their technique and watch videos to see what might be going on. During the acute phase of back pain, when someone may be limited, this is the perfect time to clear these issues up.
Manual Therapy & Modalities
There is a huge debate out there on if manual therapy and things like heat are useful or a complete waste of time. This blog is not the time to debate this, but I will say that while not the main focus of my treatment compared to education and exercise, I do use both. In the very acute phase, we are looking for any way to reduce sensitivity levels and calm down someone’s back. If 5-10 minutes. ofheat and manual therapy make a patient feel and move better, and it allows them to tolerate exercise better, I’m all for it. That said, I try to move to exercise work as fast as possible.
2. The Intermediate Phase – “Be A Human Again”
This phase of rehab, generally in the 4-6 to 10-12 week mark, is about progressing exercise programs to build local lower back and global capacity. We want to use exercise and ongoing education as our main tools to help rebuild their capacity. At this point, if workloads have been reduced and the time has been put in place, gymnasts are starting to feel a bit better. In some more significant situations, like full spondy fractures or more intense disc herniations, it might still take a bit to feel great.
Progress Core and Global Exercise
The first, and most important, task is to make the exercise program harder. This not only allows us to physically load the core and lower back structures more but also helps rebuild mental confidence. A gymnast wants to know that their back can handle harder exercises, and higher forces, without increasing symptoms. Also, sometimes loading of the lower back and core over time helps to continue to reduce sensitivity levels and fear about movements.
For this, I try to build a basic and well-balanced strength program. For the lower body patterns, I build in split squats, step-ups, single-leg hip lifts, box goblet squats, physioball curl ins, and outer hip work like sideband walks. For the core, I try to get every main core area. I like to progress the basic core work to bear crawls, wall press dead bugs, full side planks, front plank drag throughs, suitcase carries, farmer carries, and sled pushes.
Upper body strength can also be added here to round out the program. Or, if cleared and without pain, a gymnast can progress their gymnastics specific strength work in the gym. They just need to make sure that its not in the direction that triggered pain originally. I also sometimes will have a gymnast do more aerobic work like biking (for extension-based pain) or treadmill walking (for flexion-based pain).
Restore Unloaded Spine Mobility
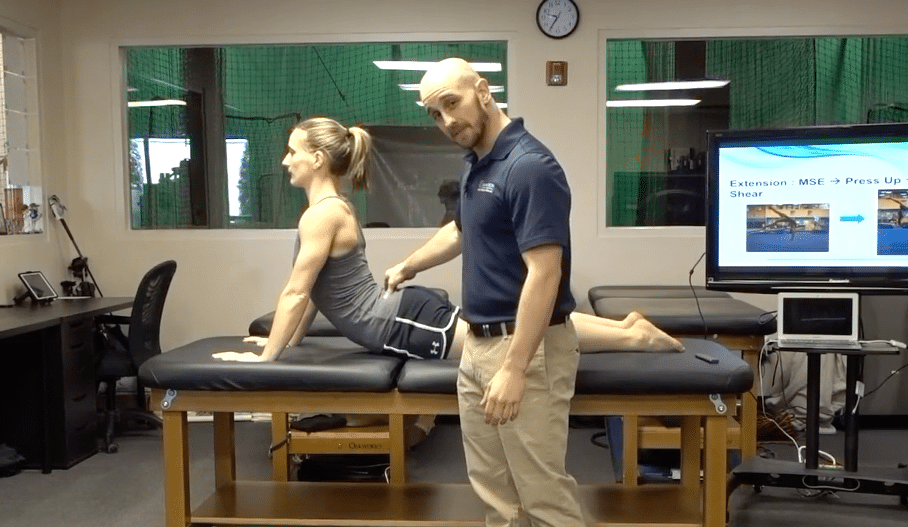
We want to make sure that we restore full lower back spine motion. For one, we want a gymnast to feel safe and comfortable knowing that they can move their spine. Along with this, gymnast requires a notable amount of lower back motion during skills. This is the first step in making sure we have this motion available so that in the next phase we can progress back to more explosive power work and basic gymnastics skills.
I use the cat camel motions in full range, press-ups, quadruped rock backs, dynamic warm-up stretches as the main way to do this. It’s normal for small amounts of discomfort, and I approach. this with a ‘consistency over intensity” mindset.
Integrate Changes Above and Below
Lastly, we want to make sure that any changes we have made to the areas above and below the lower back are used in exercise programs. We have to make sure to cue gymnasts to actively use their shoulders, thoracic spine, hips, and ankles during strength work. This allows them to rebuild movement patterns that will be used in the next few phases as they return to gymnastics.
3. The Advanced Phase – “Be An Athlete Again”
This is where things start to pick back up and get more exciting. This is during the 12-20 week phase usually, and involves much more power, speed, and gymnastics-specific work. It is crucial to note that while most gymnasts will not be in pain, or feel limited, they can not rush here. I have seen so many gymnasts try to ‘test the waters’ with skills or competing during this phse, only to flare their back up again an be really frustrated with the set back. Take it from me, go slow, and go through the proper steps. The forces of even basic gymnastics skills are massive compared to daily life. Not to mention, gymnasts have likely only had a few weeks of real strength work under their belt and may not be in peak condition for full practices/meets.
Advanced Core/Power Work

The first thing I spend a ton of time workin on is getting back advanced power and core work. Gymnastics demands a massive amount of fast twitch power output. If we never expose the lower back and core to this type of force before we reintroduce gymnastics skills, it might spike the amount of workload and bring about symptoms.
My personal favorite way of going about this is using medballs. I find that many of the movements seen in gymnastics can be trained with medicine ball throws and slams. It helps gymnasts rebuild their tolerance and comfort with fast ballistic motions, but not in gymnastics-specific settings. I use medicine ball slams, seated overhead medball throws that progress to standing overhead throws, side to side medball slams, and tall kneeling chest passes as my favorites.
Return to Jumping & Running
We also need to make sure that we return jumping, landing, and running. This is often an intimidating area for gymnasts and medical providers, but if the first few phases are done well, there is typically no issue with starting to do impact work. Keep in mind for some injuries like cartilage damage or fractures, this will take a while and will require clearance from a doctor/surgeon. These are the exercises I use to start this
- 20 Pogo hops
- 20 In and out hops
- 20 Scissor hops
- 2 laps Jogging laps forwards and backwards
- 2 laps Skipping laps forward and sideways
- 2 laps Carioca and side shufle laps
Rebuilding Gymnastics Patterns
Lastly, we need to make sure that we progress gymnasts back into the motions that their spine will experience in gymnastics. The spine of a gymnast will be exposed to unique ranges of motion we only see in gymnastics skills. So, the ability to arch, hollow, twist, and compress under load is crucial.
For this, I like doing tall kneeling backbend drills where a gymnast is encouraged to use their shoulders, thoracic spine, and hips more than their lower back for the extension. Here is a really popular video I made on that.
4. The Return to Sport Phase – “Be A Gymnast Again”
This is another very important, yet sometimes murky, area of gymnastics rehabilitation. While there has been great work by some researchers suggesting sports progressions, and other work to look at in baseball/tennis/golf, the reality is that gymnastics still largely has a lack of objective science-based return to sport protocols. Based on these tools and others, there are 3 main variables that I use to make return to gymnastics programs.
- Surface – soft surfaces like pit/trampoline, to medium surfaces like rod strips and using 8″ mats, to hard surfaces like spring floors or beams
- Force per skill – low impact force basics and drills, to moderate impact force skill or skill combination work, to high force power tumbling or vaulting or dismounts
- Repetitions – low repetitions per week, to moderate repetitions per week, to high repetitions per week

When I make these programs, I take the skills that a gymnast is currently performing and map them across the week. I have gymnasts do skill work 3 days per week, with 24 hours in between, while maintaining their strength program. I typically progress them every 2 weeks, making sure not to increase the surface demand, force per skill, and repetitions all at once. This typically looks like
- Weeks ½ – Soft Surface, Drills/Basics, Low Repetition volume
- Weeks ¾ – Soft/Medium Surface, Skills, Moderate Repetition volume
- Weeks ⅚ – Medium/hard, Harder skills, Moderate Skill Volume
- Week ⅞ – Hard Surfaces, Hard Skills, no > 7 reps per skill per day
I try to start with the skills and motions that did not originally spark their back pain. If a gymnast had extension based back pain, we may start with round-offs, jumps, leaps, and single flipping skills. Then as things progress, we will slowly add in back handsprings on tumbl trak, tap swings, strap bar, and more advanced leaps/jumps. Then, finally, in the 6+ week mark, we will do full-beam series, giants, releases, or for men’s gymnastics ring giants and bigger high bar taps.
Again, keep in mind that with mild injuries each phase may only take 1 week, totaling 4 weeks. In more severe injuries or those requiring surgeries, it may take 2-4 weeks for each phase, expanding the total time out to possible 8 or 16 weeks. While there are many caveats to these rehab programs, and individualization must always be applied based on the unique case, hopefully, these general guidelines can be useful.
What Can Be Done To Speed Up Healing in Gymnastics Back Injuries?
As I mentioned, we can’t magically eliminate the natural healing timelines of tissues. But, there are many things that we can do to assist in the healing process and help optimize the body. In my experiences, these are typically less talked about as focus points. I feel that far too many people are looking for the “best exercise” or new fads in technology to try and speed up the healing process. This typically just leads to frustrations and stalled progress. Based on the literature I have reviewed and my experiences, the biggest things we can do to assist in injury recovery are
Time
As mentioned, allowing for proper timelines of healing is crucial. We want to make sure that we apply the optimal dose of loading, followed by the optimal dose of recovery, to get tissue adaptation. If we apply too much load too soon or don’t allow enough time for recovery, we can spin our wheels and run into frustrations. As literature supports, we want to shoot for the optimal dose of stress followed by the proper period of rest for the body to heal. While this will vary from tissue to tissue (tendon vs bone vs cartilage), it still applies universally.
Sleep
Getting enough sleep, and getting high-quality sleep, are both enormously important for our body’s recovery. I refer people to some great researchers like Matthew Walker and Andrew Huberman for the great information. Some of the most common tips they suggest are
- Aiming to look at morning sunlight within the first 60 minutes of waking, and trying to see evening sunsetting light
- Having consistent waking/sleeping schedules, even on weekends
- Avoiding screens or blue light 1- 2 hours prior to bed
- Sleeping in a slightly cooler room, 68 degrees F or below
- Avoiding caffeine intake 8-10 hours before bed
- Avoiding food intake 1-2 hours before bed
Proper Fueling
Tissue healing depends on having the proper fuel sources for the body to build that tissue from. It is absolutely crucial that gymnasts are getting not only enough food intake but also high-quality ingredients, for their bodies to heal. This is not my area of expertise, but I’m lucky to be friends with some expert medical providers who specialize in nutrition for gymnasts. For more information, check out Christina Anderson, Josh Eldridge, and Kerry Blair.
Compression & Active Movement To Tolerance
As outlined extensively above, there has been a movement away from icing and into promoting movement and activity to tolerance. For those looking to help speed up the recovery process, we can try to manage the swelling, motion, and blood flow as much as possible.
Static compression garments, like compression sleeves or ace wraps, can be useful. However, intermittent pneumatic compression, say in the form of mechanical dynamic compression garments like Normatec’s, has great support in the literature to restore cellular environments for recovery. While there is not extensive medical literature on ankle injuries and compression, I do try and build it into programs when appropriate.
Proper Exercise Progressions
Above all else, we have to remember that the human body senses, responds, and adapts to the appropriate dosage of load (the geeky term being mechanotransduction). The 4 phases of rehabilitation, and all the exercises I outlined above, provide the framework for how this can be done for gymnasts with ankle and foot injuries. It’s also the reason why strength and conditioning principles are so crucial. We must be using both external weight training and body weight strength training to help increase capacity, and build a robust athlete through physical preparation.
How Do We “Prevent” Back Injuries in Gymnastics?
So with all this in mind, what can we do to stay ahead of injuries? We do have many great tools we can think apply given all this information, but it is worth noting that ‘preventing’ injuries probably isn’t realistic.
For one, injuries are extremely complex with multiple factors contributing to them. Even the best science-based “prehab’ program can address all of these.
Second, gymnastics (and all sports) are just inherently risky. There will always be bumps, bruises, and accidents that happen. While I’m certainly a fan of trying as much as we can to reduce the risk of injuries, being realistic is also important. I often don’t use the work “prevent” but more “reduce risk”. That said, let’s take a look at some evidence-based concepts that we can apply to reduce the risks of foot and ankle injuries.
Workload Planning, Management, & Monitoring
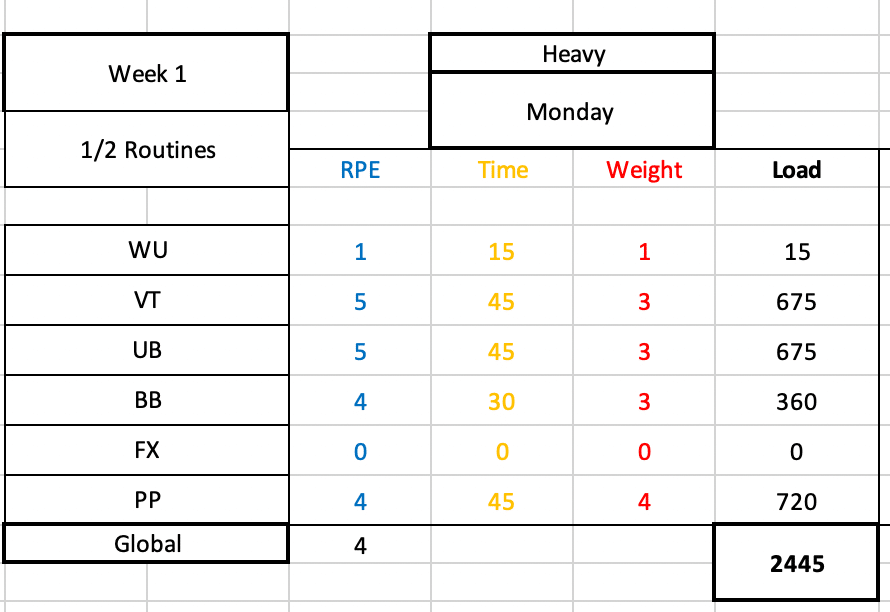
While the workload research is progressing to be less about ‘injury prevention and more about monitoring, there is great data thus far to suggest that keeping a close eye on workload can be useful.
For one, we want to make sure that we don’t subject gymnasts to rapid, unplanned, sudden spikes in impact workload. This rapid increase in load might be too much for a gymnast’s ankle/foot to handle and may contribute to elevated injury risk. This often times happens just before competition season, or when coaches might get over-excited and throw lots of new drills or plyo conditioning at gymnasts.
In another light, we also don’t want to undertrain gymnasts so that they are unprepared for the demands of gymnastics. If gymnasts are not doing an appropriate amount of skill, strength, and impact training, we may set them up for issues. Another theme in the workload research is that hard, but intelligently designed training programs, are helpful to try and reduce injury risk and increase performance.
We find the workload ‘sweet spot’ of not too much but too little, by being meticulous about the science of periodization and planning along with constant communication. We must map out the entire year, month-to-month goals, week-to-week force progressions, and daily assignments, so that we can create a progressive increase in load and back off when needed to allow recovery.
Great Strength & Conditioning Programs

This goes hand in hand with the workload concept, but formal science-based strength programs are one of the best tools that we have in helping reduce injury risk and increase performance. There is a great body of evidence suggesting that strength training, primarily with the proper usage of external weight training, is fantastic for athletes. I’m a huge fan of external weight lifting and bodyweight gymnastics being used together, in what I call ‘hybrid’ strength and conditioning programs. This is of particular importance for the lower body and foot/ankle injuries, given the forces that gymnasts experience.
Despite the overwhelming amount of evidence for the use of weight training, gymnastics culture is still largely resistant to adopting it. Many fear that it will make gymnasts ‘bulky’, lose their flexibility, or get hurt. Again, the research conflicts with this particularly when proper coaching, proper programming, and proper progression is used. For more information on this, check out this popular blog post I wrote.
Rotating Similar Types of Skills & Using Skill Caps
Another huge factor for reducing the risk of lower back pain in gymnasts is recognizing that lots of skills fall into similar movement categories. As has been outlined in depth, many skills require arching or extension. Many skills also require hollowing rounding. Many skills also put impact or compression through a gymnast’s spine.
None of these things are inherently bad, or dangerous for a gymnast. But to stay ahead of issues, it is a very good idea to plan out in advance what days you are working what motions. If a gymnast does beam series, and then tumbles on floor, and then does yurchenko vaults, and then does long hang swings on bars, those all involve arching. Similarly, if someone does impact on floor, then dismounts on bars, then dismounts on beam, and vaults to hard in the same day, this could be a lot of impact volume. By being aware of this, and planning, we can prevent spiking workloads.
Along with this, I strongly suggest that people use guideposts for how many repetitions to do. I know all too well how busy things can be on events, and saying “you have 30 minutes to do beam series” is a tempting plan. But if left open like this, gymnasts may quickly stack up 20, 30, or 50+ back bends or impacts. Instead, try to use objective markers and caps of skills. I tell gymnasts I coach now “warm-up 5 series on the lines, then try to hit 7 goood ones but don’t go over 10 attempts.” That way, we know about where we are at for volume and won’t let the train run away too fast.
Fostering Cultural Changes Around Early Specialization, Year-Round Training, and Age Guidelines
Continuing on the challenge of cultural norms, the continued focus on early specialization, year-round training, and very young gymnasts possibly being pushed too hard/too soon are huge concerns.
As with strength and conditioning, there is a massive amount of research highlighting the possible dangers of this. Both year-round training and early specialization have been associated with elevated injury risk, elevated burnout rates, and drops in long-term performance. While I do believe that there will be some lean towards earlier ages for gymnasts, particularly if they have high level goals, the tough reality is that we need to have some serious conversations about if this is beset for gymnasts’ health and long term performance.
I feel this matters most in situations like impact-based ankle/foot injuries. Doing only gymnastics from an early age, and doing it all year long, maybe subject young athletes to massive amounts of high force impact repetitions. This may create a notable risk of various injuries, and also contribute to burnout or stalled long-term performance.
Similar to this, currently are no guidelines for how many training hours per week young gymnasts of various levels should be training. How many hours per week should an 8-year-old level 6 gymnast train? What about a 13-year-old level 10? Is it ideal for the age limit of senior elite gymnastics to be 16, not 18?
I don’t have the answers to these questions. But, if we want to see actual, lasting change on the rates of ankle (and all) injuries, with higher levels of long-term performance, we must get groups of experts from all disciplines to get together and brainstorm these ideas. Particularly those around training hours, and changing our culture to not ask pre-pubertal 10-14-year-old gymnasts to be elite athletes well before they are physically or mentally ready.
Teaching Excellent Gymnastics Technique & Landing Technique
While this is not something with a ton of scientific support, it makes sense to apply the idea that a focus on excellent basics, technical foundations, and mastering proper skill progressions over multiple years is what’s best for gymnasts. During the younger years when growth and puberty are occurring, we want to help protect athletes’ bodies by teaching and using excellent techniques. This means teaching proper running, tumbling, bounding, and dismount techniques. It also means applying the best science to proper landing techniques and making sure that the judges are not deducting when athletes land properly.
This requires gym cultures that are willing and able to invest in these more ‘boring’ sides of the sport. It also requires a culture that as a whole is willing to build an educational model where coaches are required to go through academic and mentorship to learn the best practices here. We can’t just throw a bunch of drills at coaches through online forums or lectures and expect them to go back to their gym and magically know what to do. In my opinion, I think we need a 1 year combined academic/mentorship model for anyone wanting to coach gymnastics. Then, an additional 1 year of advanced course work and mentorship for those who wish to work in the higher levels of optional, college, and elite gymnastics.
Mat Usage and Surface Monitoring
Lastly, one of the major things that we can do to help reduce the risk of ankle and foot injuries in gymnastics is by utilizing the massive amount of matting technology we have at our disposal. Various sting mats, 8″ or 12″ mats, resi pits, and other devices allow gymnasts to not only train high-level skills but also compete with buffered forces. I know that financial barriers are sometimes here, but athlete safety and longevity are by far and away from the number one priority for us.
To go along with this, we must meticulously plan the progression over the competitive year from soft to semi-firm, to hard surfaces. If people think about starting to compete in December of a year, we must look backward 3 months in advance and design slow, methodical progressions from softer to harder surfaces. As we’ve seen, jumping too fast into hard surfaces without adequate time and physical preparation will significantly increase the possible injury risk. Again, education is huge here for coaches, medical providers, strength coaches, and sports scientists to all come together and create consensus statements that will help the community.
What Do We Do If Gymnast’s Back Injuries Aren’t Improving?
I would be denying the obvious if I didn’t admit that despite all the best practices, there are times when gymnasts’ ankle and foot injuries simply do not make progress. They take the appropriate time off, move through rehabilitation, and try to regain strength, but whenever they try to do their skills pain returns. In my experiences, here are the biggest factors to look into if someone can’t seem to get over their foot or ankle injury.
Culture Issues
This is by far and away from the biggest ‘elephant in the room’ issue that comes up when I work with gymnasts who seem to have long-lasting back pain. It’s crucial to make sure that the gym and community culture is not only supportive but aligned. By aligned, I mean sharing common goals.
In my experience, I find that sometimes the goals of the gymnast have changed for them to no longer want to train in a particular level of the sport, or honestly, they may not want to do gymnastics anymore. If open communication is not used, and a gymnast’s goals are not shared with parents, coaches, and medical providers, friction will result. An honest discussion about this is the first place to start if someone is struggling to get back.
Although it is less common these days, the brutal reality is that in some gyms a toxic culture exists where there is a lack of trust and athlete-centered focus. If adults are being a bit too selfish, and are not respecting someone’s injury or medical advice, they may downplay or disregard the athlete’s pain levels.
Or they may try to ‘test the waters’ on skills and go back to impact work too fast. Or, they may not be open to modifying skill profiles of gymnasts (say a less hard dismount/tumbling pass in an upcoming meet, or only doing 2 events). In some situations, gyms may not be willing to go way back to basics and correct skill techniques or get stronger as they are in season and want to rush back to competing.
When this is happening, my first recommendation is always to have a private discussion with everyone involved through the lens of empathy. Everyone likely wants the same things – for athletes, coaches, and parents to be happy and healthy. When professional discussion can occur, you can talk about the issues head-on, brainstorm solutions, and take action to change things.
If you are part of a place where someone is not open to communication or is unwilling to change, you have to ask yourself “Is this a good fit?”. Sometimes hard choices have to be made about parents, coaches, or gyms. It can be challenging, but nothing is worth sacrificing someone’s term mental or physical health.
Rehabilitation is Not Challenging Enough
Just as there can be issues with the sport and coaching side of things, there can be issues with the medical side of the fence as well. Most often, issues related to not applying the science of strength and conditioning to rehabilitation.
I find in many programs, the basic exercises that are very appropriate in the first two phases of rehabilitation never progress to advanced strength, plyometric, or power exercises. This can leave athletes short, as they are not able to rebuild their capacity. Then, once they try to go back to even basic gymnastics skills, the pain returns. Sometimes taking a step back, and really hammering strength for 4-6 weeks, is the key to getting over the hump.
In other situations, medical professionals may really lack an understanding of the sport of gymnastics. If they do not understand skill names, events, levels, and different training equipment that can be used, it might be easy to get lost. It is challenging to find medical providers who understand gymnastics, I admit this. But, thanks to the internet and many online forums, there are certainly places to develop and share this knowledge. There are also many educational platforms that can aid people in helping gymnasts more specifically.
Return To Sport Progression is Too Fast
I commonly find that the return to sports progression is too fast following back injuries. This could be due to gymnasts not feeling pain, meet season pressure, a lack of guidance, external pressure, but the reality is that if we go too fast too soon it is very easy to flare issues up.
We have to remember that once we add in more skills or training days, we are likely adding hundreds and hundreds of impacts per week. These impacts are very high force, even when basics or soft surfaces are used. In some cases with higher levels, I find that even progressing every 2 weeks for 8 weeks might be too much. We must always respect the natural adaptation process, and be understanding when someone may hit a speed bump needing to pump the breaks a bit.
Skill Technique Not Being Corrected
This is typically more on the gymnast, but it’s crucial that skill technique and landing technique be corrected if it’s an issue. Athletes who struggle with shaping positions, basic strength, tumbling mechanics, or skill foundations may have a tough time with getting back to high-impact skills. This is typically the most common for floor, vault, and dismounts.
Following injury, the ankle and feet will. be more sensitive to short landings or high forces. If someone is throwing their head out on a floor tumbling pass causing them to land short or doesn’t understand tapping mechanics to fully rotate a dismount around, this must be corrected. Without this, problems may continue to surface over and over.
Lacking Patience with Growth and Development
This last one is really more about the entire sport of gymnastics changing their perspective on the expectations we place on children in the sport. Up until the age of 16 (or more), it is a constant uphill battle against growth and development. This is a normal part of being a human that is out of the gymnast’s control. They will grow, lose flexibility temporarily, lose strength, struggle with skills, have hormonal/mental health issues, and much more.
Gymnasts are already so hard on themselves, and if an adult is lacking compassion or is putting more pressure on them, it’s a nightmare. I see this often when a young gymnast is being asked to return back quickly after an ankle/foot injury, saying they will “miss their shot” if they don’t do _______ competition. This is a really dangerous approach to take, and has to be pushed out of our sport.
Concluding Thoughts
So that brings this absolutely monstrous, epic blog post to a close. While I highly doubt that anyone read the entire thing, my hope is that you were able to jump around to get the relevant pieces of information they needed. I will continue to update this blog post over the years as I learn more, new science emerges, and I gain more experience. As mentioned above, if you want more on the topic you can check out SHIFT’s Gymnastics Strength and Conditioning Course, our monthly membership group The Hero Lab, or our full CEU approved Gymnastics Lower Extremity course for medical providers.

If there are other issues not covered here, or things you would like to learn more about, be sure to reach out to us on social media so I can put it on my to-do list!
Take care,
Dave
Dr. Dave Tilley DPT, SCS
CEO/Founder of SHIFT Movement Science
References
- Goldstein JD, Berger PE, Windler GE, Jackson DW. Spine injuries in gymnasts and swimmers. An epidemiologic investigation. The American journal of sports medicine. 1991;19(5):463-8.
- Jackson DW, Wiltse LL, Cirincoine RJ. Spondylolysis in the female gymnast. Clinical orthopaedics and related research. 1976(117):68-73.
- Micheli LJ. Back injuries in gymnastics. Clin Sports Med. 1985;4(1):85-93.
- Sands WA, Shultz BB, Newman AP. Women’s gymnastics injuries. A 5-year study. The American journal of sports medicine. 1993;21(2):271-6.
- Standaert CJ. New strategies in the management of low back injuries in gymnasts. Current sports medicine reports. 2002;1(5):293-300.
- Sward L, Hellstrom M, Jacobsson B, Nyman R, Peterson L. Disc degeneration and associated abnormalities of the spine in elite gymnasts. A magnetic resonance imaging study. Spine. 1991;16(4):437-43.
- Sward L, Hellstrom M, Jacobsson B, Peterson L. Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine. 1990;15(2):124-9.
- Hutchinson MR. Low back pain in elite rhythmic gymnasts. Medicine and science in sports and exercise. 1999;31(11):1686-8.
- Marshall SW, Covassin T, Dick R, Agel J. Descriptive epidemiology of collegiate women’s gymnastics injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. Journal of athletic training. 2007;42(2):234-40.
- Kolt GS, Kirkby RJ. Epidemiology of injury in elite and subelite female gymnasts: a comparison of retrospective and prospective findings. British journal of sports medicine. 1999;33(5):312-8.
- Kerr ZY, Hayden R, Barr M, Klossner DA, Dompier TP. Epidemiology of National Collegiate Athletic Association Women’s Gymnastics Injuries, 2009-2010 Through 2013-2014. Journal of athletic training. 2015;50(8):870-8.
- Saluan P, Styron J, Ackley JF, Prinzbach A, Billow D. Injury Types and Incidence Rates in Precollegiate Female Gymnasts: A 21-Year Experience at a Single Training Facility. Orthopaedic journal of sports medicine. 2015;3(4):2325967115577596
- O’Kane JW, Levy MR, Pietila KE, Caine DJ, Schiff MA. Survey of injuries in Seattle area levels 4 to 10 female club gymnasts. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2011;21(6):486-92.
- Vanti C., Gasperini, M., Morsillo, F., Pillastrini P., Low back pain in adolescent gymnasts. Prevelance and risk factors. Scienza Riabilitativa, 12(2) 45-50. 2010
- Fett D., Trompeter K., Platen P. Back pain in elite sports: A cross sectional study on 1114 athletes. PLOS ONE. 2017; 1-17
- Bruggermann DP Harringe ML. Biomechanics: injury mechanisms and risk factors. In Caine DJ., Russell K., Lim L. The Handbook of Sports Medicine: Gymnastics. 2013. Wiley-Blackwell: Oxford, pp 75 – 84
- Jemni, M. The Science of Gymnastics: Advanced Concepts. Routledge 2018.
- Caine D, Harringe ML. Epidemiology of injury in gymnastics. In Caine DJ., Russell K., Lim L. The Handbook of Sports Medicine: Gymnastics. 2013. Wiley-Blackwell: Oxford, pp 111 – 124
- Berger RG., Doyle SV. Spondylolysis 2019 Update. Orthopedics. 31(1) 2019.
- Yamaguchi JT., Hsu WK. Intervertebral disc herniations in elite athletes. International Orthopaedics. 2018.
- Campbell RA., et al. Injury epidemiology and risk fators I competitive artistic gymnasts: a systematic review. Br J Sports Med 2019; 0:1-15
- Goldstein JD, Berger PE, Windler GE, Jackson DW. Spine injuries in gymnasts and swimmers. An epidemiologic investigation. The American journal of sports medicine. 1991;19(5):463-8.
- Jackson DW, Wiltse LL, Cirincoine RJ. Spondylolysis in the female gymnast. Clinical orthopaedics and related research. 1976(117):68-73.
- Micheli LJ. Back injuries in gymnastics. Clin Sports Med. 1985;4(1):85-93.
- Sands WA, Shultz BB, Newman AP. Women’s gymnastics injuries. A 5-year study. The American journal of sports medicine. 1993;21(2):271-6.
- Standaert CJ. New strategies in the management of low back injuries in gymnasts. Current sports medicine reports. 2002;1(5):293-300.
- Sward L, Hellstrom M, Jacobsson B, Nyman R, Peterson L. Disc degeneration and associated abnormalities of the spine in elite gymnasts. A magnetic resonance imaging study. Spine. 1991;16(4):437-43.
- Sward L, Hellstrom M, Jacobsson B, Peterson L. Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine. 1990;15(2):124-9.
- Nusman C, van Rijn R, Lim L, Maas M. An 11-year-old high-level competitive gymnast with back pain. British journal of sports medicine. 2013;47(14):929-32.
- Ward L, Hellstrom M, Jacobsson B, Karlsson L. Vertebral ring apophysis injury in athletes. Is the etiology different in the thoracic and lumbar spine? The American journal of sports medicine. 1993;21(6):841-5.
- Chang CH, Lee ZL, Chen WJ, Tan CF, Chen LH. Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation. Spine. 2008;33(16):1750-4.
- Kadam G, Narsinghpura K, Deshmukh S, Desai S. Traumatic lumbar vertebral ring apophysis fracture with disk herniation in an adolescent. Radiology case reports. 2017;12(2):427-30.
- Wu X, Ma W, Du H, Gurung K. A review of current treatment of lumbar posterior ring apophysis fracture with lumbar disc herniation. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2013;22(3):475-88.
- Bunnell WP. An objective criterion for scoliosis screening. The Journal of bone and joint surgery American volume. 1984;66(9):1381-7.
- Coelho DM, Bonagamba GH, Oliveira AS. Scoliometer measurements of patients with idiopathic scoliosis. Brazilian journal of physical therapy. 2013;17(2):179-84.
- Hresko MT, Talwalkar V, Schwend R. Early Detection of Idiopathic Scoliosis in Adolescents. The Journal of bone and joint surgery American volume. 2016;98(16):e67.
- Patel DR, Kinsella E. Evaluation and management of lower back pain in young athletes. Translational pediatrics. 2017;6(3):225-35.
- Sweeny, et al. Returning to Sport After Gymnastics Injuries. Curr Sports Med Rep. 2018 Nov;17(11):376-390.
- Hart E., at al. The Young Injuries Gymnast: A Literature Review and Discussion. Curr Sports Med Rep. 2018 Nov;17(11):366-375.
- Gabbet, T., Debunking the myths about training load, injury and performance: empirical evidence, hot topics and recommendations for practitioners. Br J Sports Med. 2018 Oct 26. pii: bjsports-2018-099784. doi: 10.1136/bjsports-2018-099784. [Epub ahead of print]
- AIS White Paper: Prescription of training load in relation to loading and unloading phases of training. http://runpure.com.au/ais-white-paper-prescription-of-training-load-in-relation-to-loading-and-unloading-phases-of-training/
- Sands W. Injuries in Gymnastics. In Jemni M., The Science of Gymnastics: Advanced Concepts. 2018. Routledge: New York, 283 – 310
- Thomas RE., Thomas BC. A systematic review of injuries in gymnastics. The Physician and Sportsmedicine. https://doi.org/10.1080/00913847.2018.1527646
- Sgroi TA, Zajac JM. Return to Throwing after Shoulder or Elbow Injury. Curr Rev Musculoskelet Med. 2018;11(1):12-18.
- Reinold MM, Gill TJ. Current concepts in the evaluation and treatment of the shoulder in overhead-throwing athletes, part 1: physical characteristics and clinical examination. Sports Health. 2010;2(1):39-50.
- Monti R. RETURN TO HITTING: AN INTERVAL HITTING PROGRESSION AND OVERVIEW OF HITTING MECHANICS FOLLOWING INJURY. Int J Sports Phys Ther. 2015;10(7):1059-73.
- Reinold, MM. Interval sport programs: guidelines for baseball, tennis, and golf. J Orthop Sports Phys Ther. 2002 Jun;32(6):293-8.
- McGill S., Low Back Disorders: Evidence-Based Prevention and Rehabilitation. 3nd Edition. 2016. Human Kinetics : Champaign, IL.
- McGill S., Ultimate Back Fitness and Performance, 6th Edition. 2017. Human Kinetics: Champaign, Il.
- Launay F., Sports-related overuse injuries in children. Orthop Traumatol Surg Res. 2015 Feb; 101(1 Suppl): S139 – 147
- Arnold A. Overuse Physeal Injuries in Youth Athletes: Risk Factors, Prevention, and Treatment Strategies. Sports Health. 2017. 9 (2) 139 – 14
- Paterno MV., et al. Prevention of Overuse Sports Injuries in the Young Athlete. Orthop Clin North Am. 2013. October 44(4) 553 – 564.
- Chen YT, Tenforde AS, Fredericson M. Update on stress fractures in female athletes: epidemiology, treatment, and prevention. Curr Rev Musculoskelat Med. 2013. 6:173-181
- Cook JL., Rio E., Purdam CR., Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? Br J Sports Med. 2016 Oct; 50(19): 1187 – 1191
- Ardern CL, Ekås GR, Grindem H, et al 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuriesBr J Sports Med 2018;52:422-438.
- Lorenz D., Morrison S. Current Concepts in Periodization of Strength and Conditioning for the
Sports Physical Therapist. Int J Sports Phys Ther. 2015 Nov; 10(6): 734-747. - Bourdon PC., et al. Monitoring Athlete Training Loads: Consensus Statement. IJSPP 2017, 12, S2 – 161 – S2 – 170
- Brenner JS. Overuse Injuries, Overtraining, and Burnout in Child and Adolescent Athletes. Pediatrics. 2007. 119 (6)
- DiFiori JP., et al. Overuse Injuries and Burnout in Youth Sports: A Position Statement from the American Medical of Sports Medicine. Clin J Sport Med 2014; 24(1) : 3 – 20.
- Haff GG. Periodization strategies for youth development. In Llyod RS, Oliver JL, Strength and
Conditioning for Young Athletes: Science and Application. 2014. Routledge: New York. 149-158 - Turner A., Comfort P. (2018) Periodization. In Turner A, Comfort P; Advanced Strength and Conditioning: An Evidenced-Based Approach. New York: Routledge, 116 – 136
- Haff GG. The essentials of periodization. In Jeffreys I, and Moody J. Strength and Conditioning for Sports Performance. 2016. New York: Routledge. 404-448
- Gabbet TJ. (2018) Workload monitoring and athlete management. In Turner A, Comfort P; Advanced Strength and Conditioning: An Evidenced-Based Approach. New York: Routledge
- Gabbett TJ, The training – injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016. March, 50(5): 273 – 280
- Haff GG. Dispelling the myths of resistance training for youths. In Llyod RS, Oliver JL, Strength
and Conditioning for Young Athletes: Science and Application. 2014. Routledge: New York. 169 – 184