7 Steps for Overcoming Knee Pain from Osgood Schlatters in Gymnastics
Osgood-Schlatter disease is a common injury among young gymnasts, mainly caused by excessive impact forces and landing repetitions stressing the open growth plate of the knee.
It occurs when the quadriceps muscles that form the patellar tendon pull on the growth plate in the knee, causing inflammation and pain. This injury can be debilitating for gymnasts if left unchecked, leading to lots of pain but also significant lost time in the gym. Due to how common it is, and how many questions I get about it, I wanted to offer this quick blog post for parents, gymnastics coaches, and medical providers to reference should they be dealing with it.
Before I dive in, I do want to mention that for anyone in gymnastics who wants to get an insane amount of information on drills, skills, strength, culture, injuries, and more be sure to check out the 2023 SHIFT Symposium which is our massive 3 day virtual event in June! Tickets are on sale now and its shaping up to be a truly incredible weekend. Details below!
Table of Contents
How To Reduce Knee Pain in Gymnasts with Osgood Schlatters
OsGood can be extremely frustrating to deal with if the proper steps aren’t taken. I work with a lot of gymnasts who try to ‘test the waters’ prematurely and lead to bigger setbacks. As hard as it can be, patience through the steps be low really is required.
1. Reduce Impact Forces Temporarily
When someone has a flare-up of Osgood Schlatters, I first recommend to them that they plan for 2-4 weeks of reduced or no impact. People hate to hear this, but it is required to help bone inflammation resolve. Some gymnasts can get away with just doing Tumbl Trak or Trampoline and softer surfaces for a few weeks to let their knees calm down. Others unfortunately are really flared up, and have to take 2 complete weeks off from jumping, landing, and running.

2. Use Compression & Heat/Ice for Pain Management
There is a lot of debate out there about the merit of ice. My stance is that the research does support that ice may not be as useful for swelling as we once thought. But, it does serve as a powerful pain reduction agent and might be more tolerated than medicine. That said, I’ve probably reduced my use of ice by 90% in the last few years. But I do think that bone pain and really acute growth plate soreness might be a useful spot for ice. If I get someone’s pain down with small bouts of ice, and as a result that lets them exercise in PT more comfortably, I consider that a good use case temporarily.
But, I will say that generally, I find myself suggesting heat more for growth plate injuries overall. It’s all about what the patient responds to. Heat can be useful as it doubles as a way to relax the quad muscle before doing soft tissue and flexibility work to improve the range of motion.
Other efforts can be made to reduce pain or swelling by using compression, elevation, and movement to tolerance. Neoprene compression sleeves and light biking might be tolerated very well. Sometimes patellar tendon straps can be useful to take tension off the painful area, but please keep in mind these should not be used as a “quick fix” and a way for gymnasts to just keep training. In my experience, doing this just compounds the issue and makes things worse down the road.
3. Work Soft Tissue Care & Flexibility
While we don’t want to go too crazy, we do need to manage the stiffness of the quads often pulling on the knee joint. In many cases, young gymnasts are growing and this is contributing to their pain. Long bones like the femur and tibia grow much faster than the quad, hence the excessive stiffness. Soft tissue work to the quads via hands-on massage, light stretching, and light foam rolling can also be helpful in the first few weeks.
4. Slowly Rebuild Leg Strength
After pain reduces in the first 2-4 weeks without impact, local strength work should be done to help rebuild the bone’s capacity and tolerance for the load. I typically start gymnasts with exercises that are not directly loading the knee in squatting or landing-type motions. I really like single-leg hip lifts and single-leg RDL first.
Finally, we can get back to squatting motions like goblet squats, and eventually, single-leg squats to a box.
5. Maintain As Much Workloads As Safely Possible
People always ask me what still can be done in the gym, and the answer is a lot. While it won’t be a full practice due to the nature of long training hours, there is still a lot that can be done. For example, gymnasts can still do a ton of bar circuits and drill work. Regular bars, strap bars, floor bars, wall handstands, and many other things are on the table here. The key is just to not land and hop down from a bar heavy, or do dismounts.
With this, gymnasts can do tons of core and shaping work. They can work uppers, lowers, and together as well as leg lifts suspended block holds, wall-facing handstands, pike compression work, and more.
6. Slowly Rebuild Plyometrics
Once 4-6 weeks have passed of the above rest/strength work, and a gymnast is cleared by the doctor, then a return to impact can start.
It is extremely important that gymnasts reintroduce impact-based exercises first in rehab to set them up for success. I start gymnasts with 2 x 20 of pogo hops, scissor hops, skipping, running, side shuffling, etc 3x/week with 24 hours in between to monitor for pain increases.
After a few weeks and no increase in pain, I have gymnasts start back on softer surfaces like a trampoline and Tumbl Trak 3x/a week while continuing their strength work.
If this slow progression isn’t respected (yes, even in the middle of the meet season) gymnasts can struggle for years being limited by this. You have to take it week by week.
7. Slowly Return to Gymnastics Skills, Starting on Soft Surfaces
One of the most common mistakes I see in gymnastics is people who do all the right steps resting and doing exercises to help their OsGoods, but then once the pain is gone and they are ‘cleared’ they go full tilt back into hard surface impacts. I highly recommend against this.
Instead, start with 2 weeks of softer surfaces like a trampoline and Tumbl Trak, loading 2-3x/week with 24 hours in between to monitor for pain and help allow for full healing.
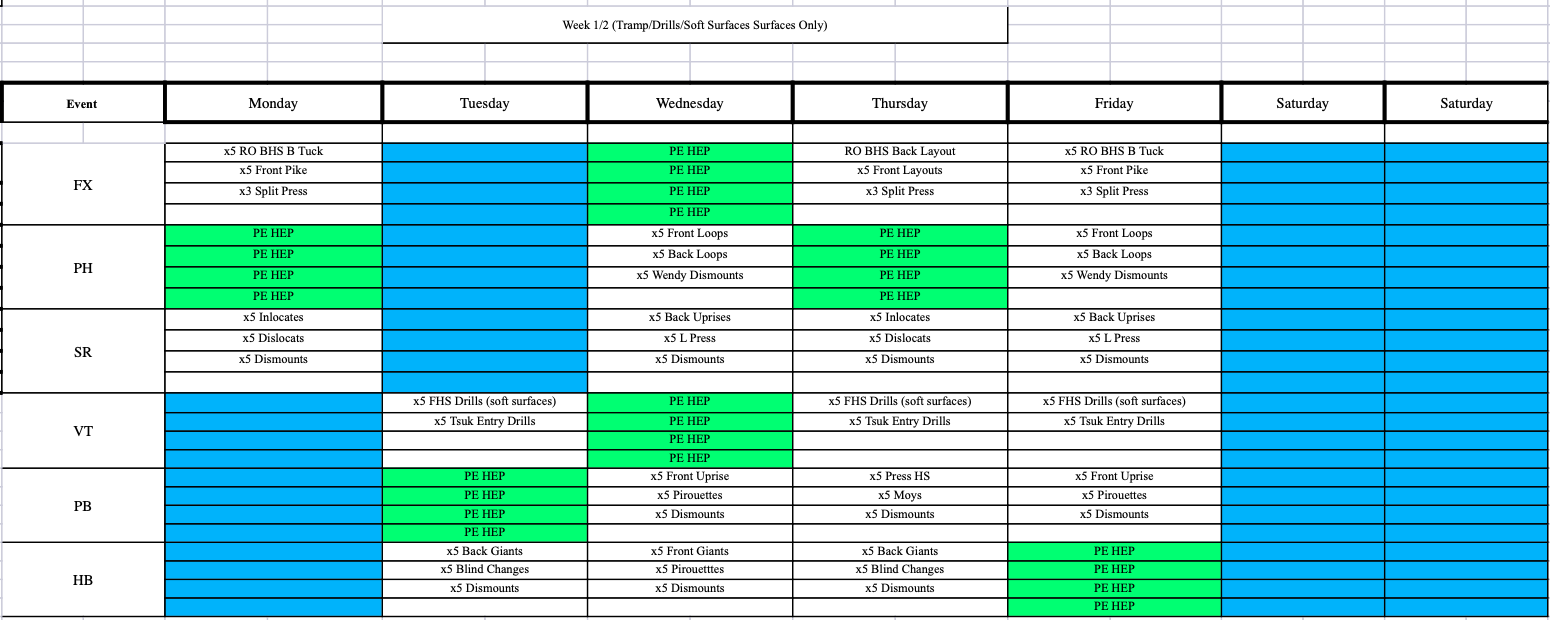
After this, 2 weeks of moderate surfaces like rod strips or landings with sting/8″ mats, and then finally back to hard surfaces with about 7 repetitions per skill being the starting point.
How Long Does It Take for Osgood Schlatters Pain to Go Away?
This is always tough to question to answer, as there are many factors to consider. If someone is aware of their knee pain early, communicates about it, and action is taken, sometimes it can be a very brief bout of 2 weeks.
On the other hand, if someone continues to try and train through pain, or does not get proper medical care early, things can get tough. I’ve had some cases of Osgood Schlatters that were so intense, the gymnast was at the point of limping or having to use crutches. It took 4 weeks of basic PT to get back to walking, followed by 4 weeks of strengthening, and 4 weeks of progressive impact work. It was 3 months before they even started Tumbl Trak and trampoline.
I say this not to scare people but to hopefully educate them. Deal with the issue head-on, early, and respect pain, and things can be much smoother. All and all I would say most cases fall right in the middle of taking 8 weeks. 2 weeks of no impact, 2 weeks of strength work, 2 weeks of power/plyo work, and 2 weeks to get back to gymnastics fully.
Concluding Thoughts
I’ll just be honest – growth plate injuries like Osgood’s are frustrating. They take lots of patience, time, and work to really get to calm down. Plus, you are always fighting an uphill battle as kids continue to grow. We have to just accept this as reality due to most athletes being younger kids in a high force, high repetition, a year-round sport like gymnastics.
If you are someone looking for an in-depth, play-by-play guide for helping with growth plate injuries in gymnastics, then be sure to sign up for the upcoming 2023 SHIFT Symposium. Due to lots of requests, we made sure to put in a great lecture on overuse knee injuries from Jan Konkle DPT OCS. You can grab your tickets here!
Have a great week,
– Dave Tilley DPT, SCS, CEO/Founder of SHIFT