5 Easy Screens for Detecting Back Pain in Gymnasts
It’s widely known that lower back pain is a huge problem in both male and female gymnastics. Despite more education coming out and progress being made, I unfortunately still treat a ton of gymnasts weekly at Champion for lower back pain. I feel by far one of the biggest contributors for things snowballing to big injuries fast is that pain is not screened for and dealt with early enough by coaches, parents, and gymnasts. Due to this, I wanted to put a post up about some quick ways a coach or gymnasts can screen for the more common form of back pain in a gymnasts. This is in an effort to hopefully catch some problems early and prevent much larger issues.

***Disclaimer***
There is a massively important disclaimer on this information: DO NOT attempt to diagnose or treat a gymnast with back pain if you are a coach/gymnast. Not only is it not in your wheelhouse of knowledge but it is also unsafe and dangerous as you could actually make them worse by recommending how to deal with the pain. There is an incredible amount of assessment and thought that needs to go into looking at a gymnast with back pain, and this post is really just one fraction of everything in an evaluation. The entire purpose of this post is to offer coaches and gymnasts a few more tools they can use to see if someone needs to hold on their gymnastics and see a doctor or healthcare provider for an evaluation. I hope that this information will be used correctly to get a gymnast early intervention should they need it, rather than having them “rest for a few days, and don’t do beam or floor” or even worse just having the athlete keep blasting away at training hoping the pain will magically disappear.
The general rule of thumb is that if a younger athlete (like a gymnast) has ongoing back pain for 3 or more days, they should be evaluated by a medical doctor and possibly get imaging to rule out a serious issue. If a gymnast takes a hard fall, lands awkwardly, or “jars” their back and complains of this type of pain they need to be cleared by a medical professional to be safe. To go along with this, I do not suggest that coaches rush to do these if someone gets hurt during practice. That is not your place as a coach and can be very, very dangerous. If these screening tests I describe below continuously provoke pain in your gymnasts lower back, I strongly suggest that the gymnast stop gymnastics and get cleared by a medical professional.
These are oriented to the more common forms of lower back problems in gymnasts (extension based/compression, pars damage, posterior spine elements, facet pathology, etc), but by no means cover everything. These movements and tests are from Stuart McGill, the SFMA model, and some other practitioners work. Others that I tend to do like the hanging test are more from my own personal experience based on working with gymnasts and knowing what might provoke pain.
1.) Standing Extension/Rotation Loading – This test comes from McGills work (also known as a quadrant test), and like those above helps to see if certain structures along one side of the posterior spine are a problem. This test has more gravity involved and tends to mimic the motions of back tumbling/extensions, etc. Have the gymnast stand up, then extend and rotate their body to one direction and reach down as if to touch the back of their knee. They will then repeat this on the other side. Make sure the gymnast move’s through their full range of motion, and have ask if they feel and pain on one side or both sides of their lower back.

2.) One Sided Prone On Elbow Extension/Rotation – Following the first screen, I like to have the athlete repeats the movement in a non gravity based position to see if they have any issues. Sometimes athletes are really good at “cheating” the screen in standing. Have the gymnast lay on their stomach, then place one arm directly underneath themselves propped up on their elbow. Have them place the other hand behind their back, then have them extend and rotate as if to look up at the ceiling. Repeat on both sides, and ask the gymnast say if/where they have pain

3.) Press Up Test (Seal Position) – These are pretty well known as movements in the gymnastics world, but they are also used to detect pain in the spine. This is a clearing test for the FMS along with a prone rocking test (cat type stretch), which can also be done. First have the gymnast press up into a full seal stretch and see if they have pain. I also tend to have the gymnast turn and look over each shoulder as well as shift their weight back and forth once at the top. I do this because these type of lateral and rotational motions while in lumbar extension are commonly seen under load in gymnastics and may cause issues.

4.) Self Compression Tests in Flexed/Extension – This is another test to see if compressive forces are problematic and may produce pain. Have the gymnast sit on the edge of a spotting block or chair. They will grab the sides of the chair/block, then pull themselves down into it. Most uses of this test have the person compress into a forward rounded posture, which definitely is important. I like to also have the athlete pull down in a slightly extended position, as this type of loading is very common for gymnasts to develop problems with due to tumbling, dismounting, and so on. I would suggest doing a rounded and extended position just to be safe.

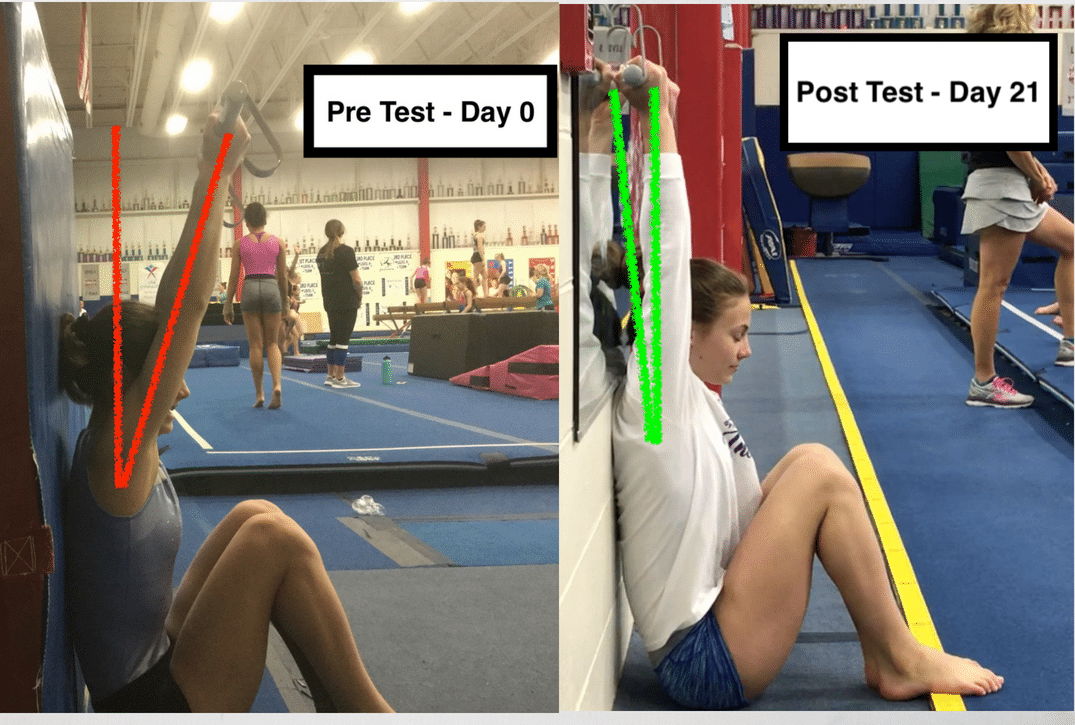
5.) Hanging Distraction Neutral and Extending – Along with compression forces in the tests above, sometimes distraction forces can be problematic with bar/ring type movements, and can also generate pain in a gymnasts’s lower back. To be completely honest, usually a gymnast has a problem with the earlier tests and I don’t actually get to doing this often. This is why I put it last, but did want to mention it. I use it more for return to gymnastics assessments. This is really a test I made off of intuition more than anything else. I first just have the gymnast hang and see if pain is present. If not, add a little bit of pulling force down to mimic the forces that go through the spine when swinging. Then, have the gymnast arch their back slightly, then again pull a little bit on their body weight.This test tends to blend between distraction forces from the bar, but also compression forces the back may take when arching during mid tap swing/giant, etc.

Important Concluding Thoughts
Now although I do want readers to use this information with their gymnasts or on themselves, please don’t dive off the cliff. Coaches I don’t advise you storm into practice saying all your gymnasts/teammates have stress fractures, because that is not the intention of this post at all. On the other side, parents reading this please do not bust down the office door of your head coach and demand everyone gets and MRI. Remember there are many different types of back pain, and a variety of different areas could be related to the issue.
I also hope this post might bring more awareness to a gymnast with pain, and that they might not want to go hero mode pushing themselves to train through pain. There are many gymnasts out there who are the ones at fault, not admitting that they have pain during training leaving coaches and parents in the dark. I want the readers of this post to be more informed and make intelligent decisions about recognizing and dealing with lower back pain early before it becomes a much more serious issue.
I can tell you first hand as a physical therapist, a coach, and a former gymnast who suffered from back pain that letting injuries go can progress quickly into bigger issues (this actually goes for many other gymnastics problems too). It can create a situation where the gymnast is forced to take many months off, possibly be put in a rigid back brace for 23 hours a day, and has a huge emotional/psychological impact on the gymnasts well being. There is nothing worse than writing off a gymnast complaining of constant pain, only to find out 3 months down the road that they are out of gymnastics with a fracture that was made worse by continuing training.
Very rarely (although possible) does one fall or skill cause a serious back injury in a young gymnast. Almost always the problem progresses over time due to their movement and training. This means that with some education and alertness from the coach/gymnast hopefully it can be picked up on with screening/early detection. If simple “rest, ice, and no tumbling for a few days” is the answer to all the gymnasts with back pain, it is likely that when they return to training the pain will creep right back up. They need a proper medical evaluation (and hopeful clearance of serious issues), and then need a movement assessment to see why they are getting the back pain in the first place.
These tests by no means encompass all the possibilities for back pain issues, and if a gymnast with back pain “clears” these tests it does not mean there is not a problem. Always, always lean on the side of caution and send the gymnast to a healthcare provider for an evaluation if they are experiencing problems. It is much better safe than sorry, and pro-active rather than reactive.
I hope that this post will not only help with some education, but also help to “catch” some back pain issues for gymnasts and get them in the right healthcare hands. Please pass this around to the coaches and gymnastics circles you know, but that’s all for now. Best of luck,
Dave
References
- Caine D., et al. The Handbook of Sports Medicine In Gymnastics. First Edition. John Wiley and Sons, 2013
- Bradshaw E.J., Hume P.A. Biomechanical approaches to identify and quantify injury
 mechanisms and risk factors in women’s artistic gymnastics. Sports Biomechanics. 2012; 11(3) 324 – 341
mechanisms and risk factors in women’s artistic gymnastics. Sports Biomechanics. 2012; 11(3) 324 – 341 - Kruse D., Lemmen B. Spine Injuries In The Sport of Gymnastics. Current Sports Medicine Reports; 8(1): January/Febuary 2009.
- McGill, S. Lower Back Disorders. Second Edition. Human Kinetics, 2007
- McGill, S. Ultimate Back Fitness and Performance: Fifth Edition. BackFitpro, Inc. 2014
- Cressey E., Reinold M., Functional Stability Training For The Core
- Cook G., et al. Movement – Functional Movement Systems: Screening, Assessment, Corrective Strategies. First Edition. On Target Publications, 2010.
- Magee D. Orthopedic Physical Assessment. Fifth Edition. St. Louis: Saunders Elsevier; 2008.