The Need to Change Landing Deductions in NCAA Gymnastics for Less Knee and Ankle Injuries
Changing how gymnasts are taught to land, in an effort to reduce the risk of serious knee injuries like ACL or meniscus tears, is something that has been talked about for the last 10+ years.
I was very grateful and humbled to be asked by the National Association of Women’s Collegiate Judging to give a presentation on what the science says is the safest way for gymnasts to land.
I gave this lecture to all the NCAA judges and NCAA coaches over two weeks. It was in an effort to help share education get everyone on the same page. But also, to hopefully change any rules around deductions that might be conflicting with what the science says is the safest way to absorb high landing forces and reduce injury risk.
Due to some copyright permission headaches, I am unable to show the full lecture in video form or use the still shots from two of vault landings I wanted. I am currently working on getting the videos swapped out and reposted, but for now, I have included some different photo examples to help. You can find the audio version of the entire lecture below as part of the podcast that went out to help people.
Due to not being able to share the video, I wanted to write this blog post summarizing the main points and highlighting examples from my presentation.
Table of Contents
Why Bother Changing Landings in Gymnastics?
So what’s the big deal anyway? Why bother going through all the headaches and fuss to change how we teach gymnasts to land?
The biggest reason is due to the massive number of serious knee and ankle injuries that gymnasts deal with, particularly in the NCAA. When you look at research studies, leg injuries account for up to 54.1% – 70.2% of all injuries (1-18).
Based on a study looking at injuries in NCAA Women’s gymnastics from 2009-2014, leg injuries accounted for 50% of all injuries with the knee and ankle being the most common (19). In some studies, up to 52% of all gymnastics injuries occur during landings, with some researchers calling it the ‘riskiest exercise phase in gymnastics.” (19-20)
What Are The Biggest Leg Injury Issues in Gymnastics?
When you dig into these studies deeper, some scary data comes out.
One of the most eye-opening takeaways from these studies is that the knee joint has the highest rate of “serious” injuries in gymnastics (18). We’re talking ACL tears, meniscus tears, fractures, and notable cartilage issues. These devastating knee injuries have the highest rates of surgery and cause the most time to be missed from gymnastics practice/competition (18).

Next to the knee joint, the ankle joint is the most commonly injured joint across all of gymnastics. Things like ankle sprains, bone fractures or chips, and cartilage damage create problems like Osteochondritis Dessicans or OCD for short (18, 21-24).
Beyond just the ‘acute’ knee and ankle injuries, it s quite clear that the overuse injury rate for the lower back, hip, knee, and ankle is astronomical across all areas of gymnastics. While this is a huge problem in NCAA gymnastics, across recreational, club, and elite levels, these injuries continue to plague gymnasts. Things like Sever’s disease, OsGood Schlatters, Ischial Apophysitis, tendonitis, shin splints, stress fractures, and more (1-17).
As much as we know these injuries can wreak havoc on a gymnast’s competitive career, the reality is that these injuries can have long-lasting consequences. We only get one spine and one set of hip, knee, and ankle joints. Many gymnasts struggle with pain or limited function well after their careers are over (25-27).
What Do All These Injuries Have in Common?
When you look at some of the common factors all these injuries share, one thing clearly sticks out – landings.

First, these injuries have many, many different factors. Second, some of them are unavoidable due to the nature of gymnastics (and all sports).
But that said, there is absolutely no denying that gymnastics landings are a HUGE common denominator for many of the severe acute and overuse injuries listed above (ACL tears, meniscus tears, ankle fractures, lower back pain, etc.)
When you look at the research around the forces of gymnastics landings, the picture becomes more clear. The forces that a gymnast’s body takes during landings can range between 5-18x bodyweight, with the highest recorded forces being at 23x bodyweight at the ankle (28-29). Not to mention, gymnasts are taking 1000s of landing repetitions per month as they learn skills, practice routines, and compete.

Given this data and the staggering number of injuries gymnasts face, it is clear that we must make sure we are doing everything we can to reduce the risk of injuries during landings.
How Do We Reduce Injury Risk AND Increase Performance?
The question then becomes, what can we do to help gymnasts reduce the risk of serious injuries?
Looking at the huge amount of scientific literature available on knee/ankle injuries in sports, there are two very impactful things that we can change (30-36)
- Using proper jumping and landing techniques, which may reduce the risk of knee injuries by up to 67% (36)
- Have a very robust strength and physical preparation program (including weight training), which may reduce the risk of overall injuries by up to 33% (37)
This is huge! We have two very evidence-based, easy-to-apply interventions for reducing the risk of devastating injuries like ACL tears, meniscus tears, and the staggering number of overuse injuries.
Not to mention, by teaching proper landing patterns and getting gymnasts as strong as possible (more below) there will be massive increases in performance by creating explosive power and increasing the chances of sticking landings. It’s a win-win.

It is absolutely crucial that coaches, judges, medical providers, and parents are all working together to get the safest possible landing patterns to be used, and then build strength in gymnasts in an effort to maximally protect themselves.
So What Landing Position Is Ideal?
Side View – More Ideal Landing
Now that we know the need to change landing patterns to the safest method possible, what is that?
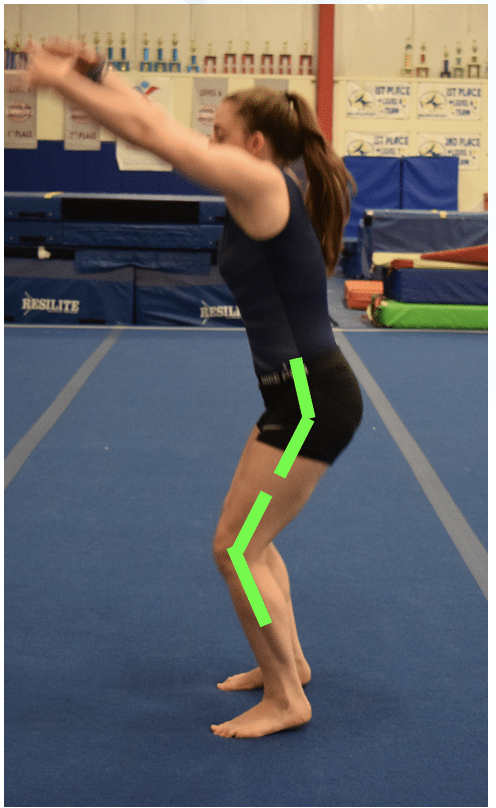
Based on an extraordinary amount of data (25, 29-43) here is the current science-supported way to land from a side profile view.
- The hip joint angle is relatively open at initial impact. Having the hip angle open allows the glutes and hamstrings to help absorb forces during the squatting motion (number 3)
- The knee joint angle is bent at 30 degrees upon initial impact. Having the knee bent at 30 degrees allows co-contraction of the hamstrings and the quads, which helps stabilize the knee joint and protect the ACL
- After the initial impact, the hip and knee joint angles bend more to a square just above parallel. This is crucial. Allowing a proper squat to parallel depth puts the glutes, hamstrings, quads, calves, and other musculature in the best possible position to disperse force through what’s called “angular displacement”. Due to the forces being so high in landings, we want to use as many muscles as possible (called dynamic stabilizers) and space the joints or ligaments (called passive stabilizers). Training a proper squatting/hinging pattern, then getting very strong in that pattern, and then using that pattern during landings, is key.
- The chest and shin lines remain relatively parallel with each other during the squat to just above parallel (with some forward chest sway being expected). There is less specific science on this concept, but we do know that we want to avoid excessive forward or low trunk lean as well as very upright torso positions. By imagining parallel lines through the shin and trunk angle, we can have about a 45-degree angle, which sets up the proper squat position above.
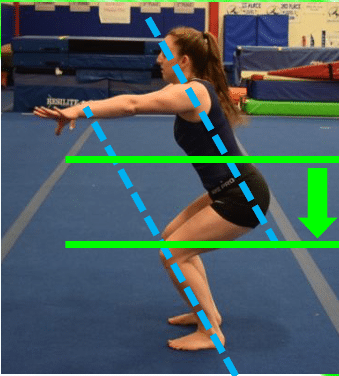
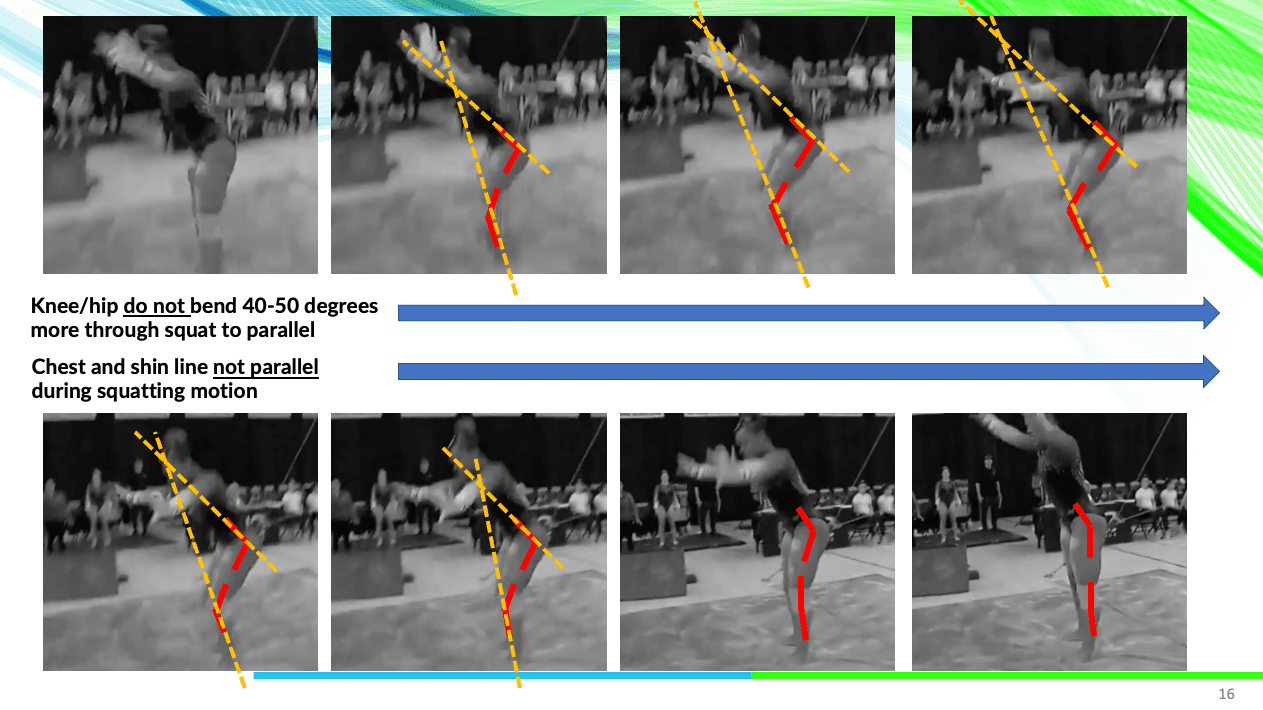
Side View – Less Ideal Landing
During my presentation to the NCAA judges and coaches, I highlighted an example of what might not be as ideal from a safety point of view. This was taken from their review of judging deductions, which I have permission to use, and you can see it below.
Some less ideal joint movements would be
- The hip joint angle is relatively closed at initial impact. A closed hip angle upon landing does not set up the ability to create more hip bending, which makes it so the larger glute max muscle can not help out as much to absorb forces.
- The knee joint angle is bent less than 30 degrees upon initial impact. When the landing position of the knee is under 30 degrees, it’s when the knee joint is most ask risk. This could be either for a ‘locked knee’ landing, but also for the quadriceps muscle to be more dominant and have less help from the hamstrings. The majority of big non contact ACL/knee injuries occur under 30 degrees of knee bending.
- After initial impact, the hip and knee joint angles do not bend more and there is a lack of squatting to just above parallel. Similar to number 1, a lack of knee bending makes it so muscles can not help dissipate forces. If we see little or no squat, also known as a ‘stiff’ landing, the glutes, hamstrings, quads, and calves can’t all work together to handle the enormous forces, which may lead to injury risk being elevated.
- The chest and shin lines remain would intersect if drawn out. If the trunk is extremely pitched forward, as in an under-rotated landing, it can be more stressful on the lower back. If the trunk is very upright and vertical, as is commonly taught in some areas of gymnastics, it might place significantly more stress on the knee and ankle joints.
Here is a video that I was allowed permission to use during the judging/coaching sessions, in an effort to help visualize these points.
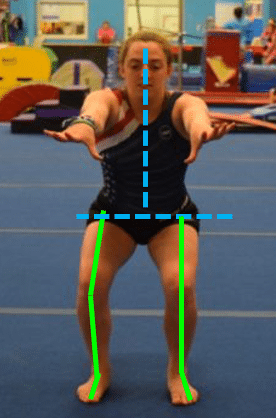
Front View – More Ideal Landing
What about from the front? Now that we have the side organized, let’s see what the front position should look like. There are really two main things to focus on
- The hips, knees, and ankles all remain in line throughout the squatting motion. The is one of THE most important things for landings in gymnastics. We want to see the legs move in a ‘train tracks” pattern so that the outer hip muscles can be in the best possible position to prevent the knees from caving in. This caving in effect also called a dynamic valgus, is one of the main contributing factors to ACL tears, meniscus tears, and bone stress injuries.
- The chest is centered over the middle of the body, with equal weight through each leg. As mentioned above, the forces of gymnastics landings can be up to 18x bodyweight. By keeping the chest centered over both legs, we can try to spread the landing forces out 50/50 into both legs.
Front View – Less Ideal Landing
And just to round things out, let’s make sure we mention what might be less ideal front the front view.
- The feet are within hip width upon impact. This is a big one that still needs to change in gymnastics. If the feet are together, it makes it much harder for the leg musculature and the outer hip muscles to help control the pivoting/twisting actions at the knee during landings. Particularly in a sport where twisting happens all the time, and people may be landing without full twists completed, we really want the feet to be hip-width.
- The feet are very far outside hip-width upon impact. Similarly, if the feet land excessively far outside the hip width, the ground reaction forces make it more likely for the knees to cave in towards each other. We also don’t want this to happen.
- The knees ‘cave’ in towards each other during force absorption. This goes without saying, but even if someone does land with the feet in the proper position, the knees may still quickly cave in. This can happen extremely fast, where the knees knock together and is often called a ‘valgus twitch’ by some medical professionals. We want the legs to remain fully in line throughout the entire descent and ascent of the landing process.
- The chest leans over one leg more than the other. If the chest is leaning excessively over one side of the body, it can cause a disproportional amount of force to go through one leg, and lead to elevated injury risk. Not to mention, excessive trunk lean over one knee can throw off the landing movement, and possibly push the knees inward.
Here is another example of less ideal ‘front’ view landing mechanics. It is challenging to see, but if you look quickly we see that the right knee quickly caves in and the body is leaning more over the left leg.

Also, here is a useful ‘summary’ slide that outlines the less ideal and more ideal landing patterns for gymnasts.

Why Gymnasts Should Lift Weights
Quickly, it’s important to reiterate that the best landing mechanics in the world won’t be enough to substantially reduce injury risk. There are many other factors, some that are not modifiable, that we have to remember.
That said, proper strength and conditioning programs that use external weight lifting are supported to have a massive impact on reducing injury risk. I think the lower body and landing injury risk is one of the clearest examples of this.

It’s why I’m a massive fan of gymnastics culture changing to support gymnasts lifting weights, as I’ve been pushing for the last 5-10 years. A properly done weight training program that uses the proper sets, reps, exercise, coaching, and programming can not only massively skyrocket a gymnasts’ strength and power, it can also substantially build capacity to help handle landing forces.
Now, it’s important to also note that I am a huge fan of traditional bodyweight exercises for gymnasts. These are staples and must be done on a daily basis. It’s not about not doing bodyweight exercises. It’s about combining the best of both worlds, and doing what I call a ‘hybrid’ model of gymnastics strength and conditioning. It will always have a combination of weight training and bodyweight work, biasing one or the other based on the time of the competitive season and the periodization plan.
Many people may be wondering what the best lower body strength exercises are to not only increase power but also reduce the risk of landing injures. Based on the literature and my 10 years helping gymnasts build these programs, some of the most helpful exercises I’ve found are.
- Weighted hip lifts
- Trap bar deadlifts
- Single-Leg Romanian deadlifts
- Split Squats
- Step-Ups/Step Downs
- Goblet Squats/Front Squats
- Farmer and Suitcase Carries
If you haven’t already tried to work these into your programs, I strongly suggest you learn a bit, or work with a Certified Strength Coach. It can provide insane benefits to gymnasts you work with.
Concluding Thoughts
I’ll leave everyone with 3 concluding thoughts based on everything above.
- We want to teach, use, and encourage the safest possible landing strategy based on the current science and then get incredibly strong to build capacity
- Traditional landings with a more upright torso, knees together, less squat depth, etc may look better to some… but science says they are not the safest
- Adopting the more ideal, science-supported, landing style sport wide will help gymnasts reduce their risk of serious injuries AND increase their chances of sticking\
It’s also really important to mention that these changes must be adopted sport-wide. The most important time to teach these proper landings are when gymnasts are very young, and just starting out. It’s crucial that we adopt these changes in deductions, as well as teaching the proper way to land, from the recreational level, to the age group/club level, through the elite code, and into NCAA gymnastics.
Here is the full lecture that I did, in audio version for now, with all of the NCAA judges and coaches if you wish to listen to it, and below you can find all of the scientific references mentioned above.



I hope this was helpful, and please share it with your community if you found it to be useful!
– Dave
Dr. Dave Tilley DPT, SCS
CEO/Founder of SHIFT Movement Science
References
- Bak K, Kalms SB, Olesen S, Jargensen U. Epidemiology of injuries in gymnastics. Scand J Med Sci Sports. 1994;4(2):148–54.
- Harringe ML, Lindblad S, Werner S. Do team gymnasts compete in spite of symptoms from an injury? Br J Sports Med. 2004;38(4):398–401.
- Snook GA. Injuries in women’s gymnastics. A 5-year study. Am J Sports Med. 1979;7(4):242–4.
- Pettrone FA, Ricciardelli E. Gymnastic injuries: the Virginia experience 1982–1983. Am J Sports Med. 1987;15(1):59–62.
- Meeusen R, Borms J. Gymnastic injuries. Sports Med. 1992;13(5):337–56.
- Hudash GW, Albright JP. Women’s intercollegiate gymnastics injury patterns and permanent medical disability. Am J Sports Med. 1993;21:314–20.
- O’Kane JW, Levy MR, Pietila KE, Caine DJ, Schiff MA. Survey of injuries in Seattle area levels 4 to 10 female club gymnasts. Clin J Sport Med. 2011;21(6):486–92.
- Dixon M, Fricker P. Injuries to elite gymnasts over 10 yr. Med Sci Sports Exerc. 1993;25(12):1322–9.
- Garrick JG, Requa RK. Epidemiology of women’s gymnastics injuries. Am J Sports Med. 1980;8(4):261–4.
- Weiker GG. Injuries in club gymnastics. Phys Sports Med. 1985;13(4):63–6.
- Caine D, Knutzen K, Howe W, Keeler L, Sheppard L, Henrichs D, et al. A three-year epidemiological study of injuries affecting young female gymnasts. Phys Therap Sport. 2003;4:10–23.
- Lindner KJ, Caine DJ. Injury patterns of female competitive club gymnasts. Can J Sport Sci. 1990;15(4):254–61.
- Kolt GS, Kirkby RJ. Epidemiology of injury in elite and subelite female gymnasts: a comparison of retrospective and prospective findings. Br J Sports Med. 1999;33(5):312–8.
- Caine D, Cochrane B, Caine C, Zemper E. An epidemiologic investigation of injuries affecting young competitive female gymnasts. Am J Sports Med. 1989;17(6):811–20.
- Steele VA, White JA. Injury amongst female gymnasts. Proceedings of the Society of Sports Sciences: Sport and Science Conference; Liverpool, School of Physical Education and Recreation; 1983.
- Kolt GS, Kirkby RJ. Epidemiology of injury in Australian female gymnasts. Sports Med Train Rehabil. 1995;6(3):223–31.
- Kerr G, Minden H. Psychological factors related to the occurrence of athletic injuries. J Sport Exerc Psychol. 1988;10(2):167–73.
- Kerr ZY, Hayden R, Barr M, Klossner DA, Dompier TP. Epidemiology of National Collegiate Athletic Association Women’s Gymnastics Injuries, 2009–2010 Through 2013–2014. J Athl Train. 2015;50(8):870–8.
- Harringe ML, Renstrom P, Werner S. Injury incidence, mechanism and diagnosis in top-level teamgym: a prospective study conducted over one season. Scand J Med Sci Sports. 2007;17(2):115–9.
- Sweeney, et al. Gymnastics Medicine. Lower Extremity Injuries in Gymnastics. Switzerland, Springer, 2020.
- Hunt KJ, Hurwit D, Robell K, Gatewood C, Botser IB, Matheson G. Incidence and epidemiology of foot and ankle injuries in elite collegiate athletes. Am J Sports Med. 2017;45(2):426–33.
- Cupisti A, D’Alessandro C, Evangelisti I, Umbri C, Rossi M, Galetta F, et al. Injury survey in competitive sub-elite rhythmic gymnasts: results from a prospective controlled study. J Sports Med Phys Fitness. 2007;47(2):203–7.
- Marshall SW, Covassin T, Dick R, Nassar LG, Agel J. Descriptive epidemiology of collegiate women’s gymnastics injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):234–40.
- Singh S, Smith GA, Fields SK, McKenzie LB. Gymnastics-related injuries to children treated in emergency departments in the United States, 1990–2005. Pediatrics. 2008;121(4):e954–e60.
- Wilk KE, Arrigo CA. Rehabilitation Principles of the Anterior Cruciate Ligament Reconstructed Knee: Twelve Steps for Successful Progression and Return to Play. Clin Sports Med. 2017 Jan;36(1):189-232. doi: 10.1016/j.csm.2016.08.012. PMID: 27871658.
- MOON Knee Group, Spindler KP, et al. Ten-Year Outcomes and Risk Factors After Anterior Cruciate Ligament Reconstruction: A MOON Longitudinal Prospective Cohort Study. Am J Sports Med. 2018 Mar;46(4):815-825. doi: 10.1177/0363546517749850. PMID: 29543512; PMCID: PMC6036619.
- Maffulli N, et al. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010 Jan;44(1):21-5. doi: 10.1136/bjsm.2009.069526. Epub 2009 Dec 1. PMID: 19952376.
- Brüggemann GP. Biomechanics of gymnastic techniques. Sports Sci Rev. 1994;3(2):79–120.
- McNitt-Gray J, editor. The influence of joint flexion, impact velocity, rotation, and surface characteristics on the forces and torques experienced during gymnastics landings. Federation International de Gymnastics Scientific/Medical Symposium Proceedings; 1991; Indianapolis, IN: USA Gymnastics.
- Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature – part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(1):69-78. doi:10.1177/1941738111428281
- EmerSmith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature – part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(1):69-78. doi:10.1177/1941738111428281
- y CA,et al. Neuromuscular training injury prevention strategies in youth sport: a systematic review and meta-analysis. Br J Sports Med. 2015 Jul;49(13):865-70. doi: 10.1136/bjsports-2015-094639. PMID: 26084526
- Nessler T, Denney L, Sampley J. ACL Injury Prevention: What Does Research Tell Us?. Curr Rev Musculoskelet Med. 2017;10(3):281-288. doi:10.1007/s12178-017-9416-5
- Ardern CL, et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Knee Surg Sports Traumatol Arthrosc. 2018 Apr;26(4):989-1010. doi: 10.1007/s00167-018-4865-y. Epub 2018 Feb 17. PMID: 29455243; PMCID: PMC5876259.
- Boling MC, et al. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009 Nov;37(11):2108-16. doi: 10.1177/0363546509337934. Epub 2009 Sep 24. PMID: 19797162; PMCID: PMC2860575.
- Webster KE, Hewett TE. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res. 2018 Oct;36(10):2696-2708. doi: 10.1002/jor.24043. Epub 2018 Jun 13. PMID: 29737024.Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014 Jun;48(11):871-7. doi: 10.1136/bjsports-2013-092538. Epub 2013 Oct 7. PMID: 24100287.
- Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014 Jun;48(11):871-7. doi: 10.1136/bjsports-2013-092538. Epub 2013 Oct 7. PMID: 24100287.
- Root H, Trojian T, Martinez J, Kraemer W, DiStefano LJ. Landing Technique and Performance in Youth Athletes After a Single Injury-Prevention Program Session. J Athl Train. 2015;50(11):1149-1157. doi:10.4085/1062-6050-50.11.01
- Escamilla RF, et al . Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weight-bearing exercises: a guide to exercise selection. J Orthop Sports Phys Ther. 2012 Mar;42(3):208-20. doi: 10.2519/jospt.2012.3768. Epub 2012 Feb 29. PMID: 22387600.
- Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006 Mar;34(3):490-8. doi: 10.1177/0363546505282619. Epub 2005 Dec 28. PMID: 16382007.
- Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012 Mar;42(3):153-71. doi: 10.2519/jospt.2012.3741. Epub 2012 Feb 29. PMID: 22382825.
- Hewett TE, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005 Apr;33(4):492-501. doi: 10.1177/0363546504269591. Epub 2005 Feb 8. PMID: 15722287.
- Podraza JT, White SC. Effect of knee flexion angle on ground reaction forces, knee moments and muscle co-contraction during an impact-like deceleration landing: implications for the non-contact mechanism of ACL injury. Knee. 2010 Aug;17(4):291-5. doi: 10.1016/j.knee.2010.02.013. Epub 2010 Mar 29. PMID: 20303276.
- Yavuz HU, Erdag D. Kinematic and Electromyographic Activity Changes during Back Squat with Submaximal and Maximal Loading. Appl Bionics Biomech. 2017;2017:9084725. doi: 10.1155/2017/9084725. Epub 2017 May 4. PMID: 28546738; PMCID: PMC5435978.
- Caterisano A, Moss RF, Pellinger TK, Woodruff K, Lewis VC, Booth W, Khadra T. The effect of back squat depth on the EMG activity of 4 superficial hip and thigh muscles. J Strength Cond Res. 2002 Aug;16(3):428-32. PMID: 12173958.