Combatting Achilles Tears in NCAA Gymnastics (Part 1)
Table of Contents
Introduction
Achilles injuries, and more specifically Achilles tendon ruptures, have come to light as a massive problem in NCAA gymnastics. They exist on the men’s side, but are clearly a bigger issue within the women’s artistic world. Although the rates of tears are high in the last few years, this has been an ongoing problem for the last decade.

Current research supports this trend. This recent 2020 study looked at the rates of Achilles injuries in 16 NCAA sports from 2005 – 2016. It showed that out of 255 injuries, women’s gymnastics had one of the highest rates. It was not said what Division these schools were, and obviously this study didn’t include the entire range of NCAA gymnastics teams, but it is still a significant finding.
The noted injury rate for women’s gymnastics was the highest of all sports at 16.73 per 100,000 exposures for all Achilles injuries. The sport in second to gymnastics was 4.26 for men’s basketball, with a notable drop in rates. This was also true for severe Achilles injuries (such as tears) that were season-ending or required surgery. The severe Achilles injury rate was noted at 7.87 per 100.000 exposures for women’s gymnastics. Men’s indoor track did have a higher rate at 11.06, but gymnastics was the highest for women’s sports.
Even more worrisome is that these problems exist at the younger levels. People are quick to blame the NCAA for all the issues, claiming ruptures don’t happen in younger athletes but hat isn’t entirely true. There are problems with ruptures before college. I hear about high school aged gymnasts suffering Achilles ruptures each year via email and message. I’m also currently treating two 16-year-old level 10’s who are still recovering from their tears during the end of the 18-19 season.
Outside of just ruptures, we have to remember there are huge rates of other Achilles injuries in youth gymnastics. One reason we don’t see Achilles ruptures as commonly in the younger ages leading up to about age 15, is because the Achilles tendon is not the ‘weakest link’. In ages under 15, most gymnasts are still going through puberty. In this age range, the bone of the heel is not fully formed, so it takes the brunt of the force, leading to a condition called Sever’s disease (research here and here)
As the gymnast matures and the boney growth plate fuses, the stress then shifts to the Achilles tendon, which is where issues may start to come up. There are a lot of high school aged gymnasts who struggle with Achilles tendinopathy and chronic calf strains. As I will discuss below, there may be a link between Achilles issues in younger years (Severs, Achilles tendinopathy, chronic calf strains) and future risk of rupture. I’m not suggesting causation, and I’m not saying there aren’t factors in the NCAA, but we have to look at everything.
After hearing about 20 Achilles tears in the first 4 weeks of the 2020 NCAA season, I really wanted to try and offer some information on the scientific literature, my thoughts on why the Achilles tear rates are so high, and what we all may be able to do about it.
In this article, I will share ideas from the latest research, and then offer some thoughts on what it means for gymnastics. This will be Part 1 of the article, as I am going to be chatting with a world-leading expert in tendon issues soon. That discusison and my expanded thoughts on it will be Part 2.
I always like to take the path of doing the work to read, learn, and form opinions for myself so I can better understand things. But I’m more than happy to be wrong and learn. I’ll be sure to update any points after talking with some experts in the tendon field.
Lastly, if you would rather listen to this vs read, I also released it in podcast form and you can find it on iTunes, Spotify, or Stitcher here.
Combatting Achilles Tears in NCAA Gymnastics (Part 1) – Podcast Audio
Achilles Tear Research Review
I took a deep dive into the literature from the last 10 years. I wanted to refresh myself from the first time I looked at this problem in 2014 (Part 1 and Part 2). I also wanted to learn more and update anything I may have been wrong about.
Out of the 50 or so research articles I narrowed in on, I ended up reading 19 articles that were directly useful. I wanted to include the most relevant points from 6 of them here, as they relate the most to practical ideas for changes in gymnastics.
Keep in mind, almost all of the patients in these articles skewed to be males and older than NCAA gymnasts (most in the 25-50 age range). This is a big factor when we talk about external validity, or the ability to generalize the results to women’s NCAA gymnastics.
Be warned, the first half of his blog is the mega geeky covering histology and pathophysiology. If this isn’t your avenue and you are looking for for just relevance to gymnastics, jump to the next section.
Articles
Click here for article – https://www.ncbi.nlm.nih.gov/pubmed/31370991
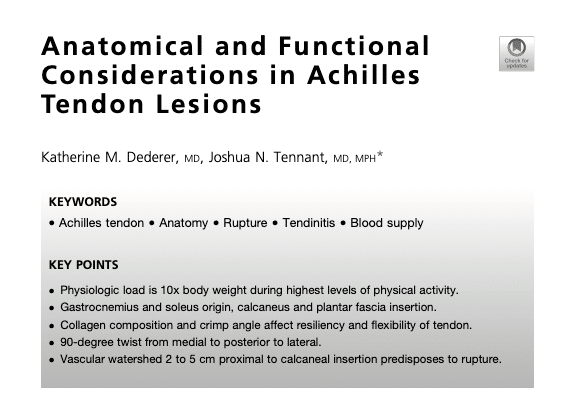
Important Information – This was a review of Achilles anatomy/functional biomechanics. It’s critical to understand the healthy tendon before we start diving into pathological findings.
- A dual blood supply exists for the Achilles tendon, which creates a watershed region which may predispose injury
- With age or during healing periods of recovery, the mechanical properties of the Achilles change as well as collagen composition, which may create risk of rupture
- Achilles rupture tends to occur 80% of the time between 2cm – 6cm proximal to the calcaneal insertion
- Ruptures typically occur when a stretch of greater than 8% occurs (but might be different for healthy vs primed pathological tendons)
- The healthy Achilles is 95% Type I collagen, with a parallel configuration and covalent bones between fibrils that give high tensile strength
- Ruptured and tendinopathic tendons tend to show a decrease in Type I collagen and increase presence of Type III collagen
- Type III collagen yields lower tensile strength and therefore may predispose rupture.
- Type III collagen tends to appear as repetitive microtrauma to the tendon occurs without proper healing timeline, rehab, or inadequate recovery environment exists, resulting in degenerative tendon states
- The size of Achilles tendon fibrils has been shown to correlate with the risk of tendon rupture.
- Tendons containing shorter fibrils and decreased fibril wideth correlate with risk of rupture
- Many studies discussing fibrils are done in animals, not humans, so we need to take findings with a grain of salt
- The % of Type I collagen, fiber density, and fiber diameter reduce with age.
- Crimp tissue acts as a buffer against rupture injury from sudden stretch. Crimp angle tends to be decreased in ruptured tendons compared to controls
- Achilles tendinopathy increases tendon diameter, and ruptured tendons tend to be significantly wider than controls, which occurs due to repetitive microtrauma
- As the Achilles tendon thickens, it’s ability to glide in the paratenon becomes impaired
Click here for article – https://www.ncbi.nlm.nih.gov/pubmed/31978571
Important Information – This was another comprehensive anatomy review of the Achilles tendon
- The fibers of the Achilles twist 90 degrees moving medial to posterior to lateral, allowing for stored energy to be used during locomotion (also mentioned in article above)
- Macrocirculation from dual blood supply, and microcirculation at the local tendon, may play a role in tendinopathy (which may precede and influence rupture risk)
- Neovascularization of the microcirculation of the Achilles has been closed related with tendinopathy, which may impact the ability to heal tissue after high load
- Tendons impacted by tendinopathy show increased blow flow due to neovascularization, which may be useful for ultrasound detection of risk
- Variable vascularization of the mid-portion of the tendon may play a crucial role in Achilles rupture risk, as this impacts the mechanical durability of the tendon
- Collagen constitutes 65%-80% of dry mass of healthy tendons, a variety of different collagen types support mechanical properties
- The Achilles tendon is composed of typical connective tissue and has a hierarchical structure composed of Type I collagen with fiber bundles, fascicles, and fibrils, as well as proteoglycans (mainly decorin and fibromodulin)
- This study reports 90% Type I Collagen in the Achilles (vs 95% above)
- Besides collagen, elastin provides mechanical properties of tendons despite only being 1% of total dry weight
- Proteoglycans (PG) and non-collagenous glycoproteins are also in the matrix, and along with structural and regulatory function, they provide control of proliferation, differentiation, migration, and survival of tenocytes
- The presence of large quantities of the glycoprotein fibronectin within a tendon may be a symptom of tissue degeneration
- In cases of tendinopathy and rupture of the Achilles tendon, tenocytes produce much more type III collagen, and the tendon becomes less resistant to tensile forces
- In tendinosis, one may see disorientation of collagen organization, separation of fibers, increase in the content of basic synovial substances
- Pathological changes that occur in tendinopathies cause instability in the structure of the Achilles tendon and disturb it’s mechanical properties
- During running the Achilles tendon experiences loads over 12x body weight (basic tumbling has shown up to 15x, unkown for higher level skills and short landings/steep take off angles in tumbling)
Click here for article – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5867427/pdf/bjsports-2017-098161.pdf
Important Information – This study looked at the Achilles tendons of people with tendinopathies and ruptures for patterns in the tissue, and compared it to the person’s healthy hamstring tissue. 7 females and 10 males aged 41-71 with tendinopathies, 4 females and 15 males ages 20-67 with ruptured Achilles
- Ruptured tissue showed evidence of chronic (non-resolving) inflammation (CD206 and CD T63 markers)
- Tendinopathic and ruptures Achilles showed higher levels of inflammatory markers CD14+ and CD68 as well as a complex inflammation signature including NF-kB, interferon, and STAT-6
- Achilles ruptures expressed increased PTGS2 and interleukin-8 expression, and both showed stromal fibroblast activation markers
- Proliferation markers and fibroblasts are likely due to microtrauma and an attempt to heal
- Resident stromal fibroblasts from diseased tendons show a pro-inflammatory phenotype
- Inflammation is a feature of both mid-portion Achilles tendinopathy and rupture
- Ruptured Achilles tendons highly expressed NF-kb target genes PTGS2 and IL-8 (a significant promoter of angiogenesis) and showed increased vascularity
- Keep in mind the differences in inflammation signatures are likely a result of recent trauma in earlier clinical presentations of Achilles ruptures
- Diseased Achilles tendons undergo phenotype change and may become primed after exposure to inflammation
- Primed tenocytes can become chronic inflammatory fibrosis tissues if not given the proper recovery and healing environment
- Chronic inflammation and fibrosis develop due to impaired resolution of inflammation and a failure to clear apoptotic cells
Click for article – https://www.hindawi.com/journals/bmri/2018/2367615/
Important Information – This study used an advanced imaging technology called ASE (Axial-strain elstography) to compare the injured torn Achilles compared to the other non injured in tact Achilles tendon as well as healthy controls. 33 patients (27 male and 6 female, ages 25-65) were compared to 19 healthy controls (14 male and 5 female, ages 25-58)
- This study references another study of 397 biopsies from recently ruptured Achilles. Those patients showed degenerative alterations of biomechanical properties such as hypoxic degeneration, mucoid degeneration, tendonlipomatosis, and calcifying tendinopathies
- These histopathological changes may alter the physical properties of the Achilles tendons like hardness (the ability of a material to resist plastic deformation)
- Hardness can be represented as strains quantitatively, which can be detected via axial-strain sonoelastography (ASE), a form of ultrasound
- At transversal scans, in the proximal third of the tendon body in study groups were significantly smaller than those in control groups
- This indicates that the proximal third tendons in the study group were softer than those in the control group
- Compared to asymptomatic tendons in normal volunteers, two morphological variables (thickness and cross-sectional area) of asymptomatic tendons in rupture population were larger
- The eccentricity of the study group was also closer to 0, revealing that the tendons from the study group were thicker, larger, and rounder than those of healthy control groups, especially in the middle
- Another study references discussed how the normal tendon is typically hard, where 57% of the tendons with symptoms of tendinopathy showed marked softening
- This may be an indicator of pathology and changes in the mechanical properties / structural integrity, which can impact risk of rupture
- Another study by Chen et al also demonstrated significant softening of the completely ruptured Achilles tendons compared to normal tendons
- Increasing hardness is found during recovery after rupture, and increasing hardness is correlated to decreasing Bonar scales under a microscope, indicating a less pathological state
- Bilateral softening was found in subjects who had a unilateral Achilles tear, suggesting morphological changes in asymptomatic tendons to look at proactively
- Overall, the important finding is that Achilles tendons on the asymptomatic side in patients with acute rupture previously were thicker and larger than healthy controls at teh middle and distal third
- Chronic exposure to repetitive loading would result in the enlargement of cross-sectional areas of Achilles tendons
- Hard to tell if the morphological changes were contemporaneous changes during the development of ruptures or an adaptation outcome of overload and overuse
- Evidence from the asymptomatic, non injured contralateral tendons showed evidence of microtrauma and healing states despite being intact clinically
Click for article – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5855626/pdf/ijms-19-00404.pdf
Important Information – Achilles tendon samples were taken from patients with chronic tendinopathy (n=7), chronic ruptures (n=6), acute ruptures (n=13) and intact tendons (n=4) looking for histological scores and pathological changes
- Pathological changes were significantly increased in tendinopathy and chronic rupture compared to acute rupture
- PCE analysis revealed significantly altered expression of genes related to collagens and matrix modeling/remodeling in tendinopathy and chronic ruptures compared to intact tendons and/or acute ruptures
- All three tendon pathology groups had markers of inflammation (interleukin (IL) 1B, tumor necrosis factor alpha, IL6, IL 10, IL33, soluble ST2) and inflammatory cells (CD3, CD68, CD80, CD206) and innervation but only significantly in acute ruptured tendons
- Tendinopathic tendons tend to show excessive proliferation of tenocytes, changes in tenocyte morphology, disruption of collagen fibers, increase in non-collagenous matric such as glycosaminoglycans (GAGs) and fat tissue as well as neovascularization
- The presence of inflammatory cells in tendinopathic states is still up for debate
- Tendon architecture was found to be fully disoriented in all acutely ruptured tendons
- Increase collagenase MMP1 was found in ruptured tendons
- Reduced IL33 was found in acute ruptures compared to tendinopathic samples
- Overall, the acutely ruptured tendons showed the strongest alterations compared to the intact tendons for nearly all analyzed processes – modeling/remodeling, inflammation, immune cells, fatty infiltrates, and innervation
- Inflammation markers may be less important in acute ruptures due to the recent traumatic tissue environment
Click for article – https://www.ncbi.nlm.nih.gov/pubmed/31385834
Important Information – This article reviewed studies investigating asymptomatic tendon changes on imaging in athletes
- Notable findings for the asymptomatic Achilles tendon were neovascularization, hypoechogenicity, and tendon thickening
- The role of neovascularization is debated, with conflicting results in studies. One study did show runners had a 7x increase risk of future tendinopathy with neovascularization shown on prior asymptomatic US
- Runners with a history of contralateral Achilles tendon rupture demonstrated significantly increased neovascularization in the uninjured tendon on CEUS (but not Doppler)
- Neovascularization in the Achilles tendon is still considered a significant risk factor for future symptom development
- Alterations in tendon structure also have been noted in asymptomatic Achilles tissue, and US studies showing areas of hypoechogenicity and tendon thickening, particularly when spindle-shaped and being associated with the development of pain in other populations
- Increase tendon thickening has also been noted as a finding, but this may be a normal response to loading
- Prophylactic eccentric exercise regimens were found to reduce the risk of patellar pain, but not for Achilles pain. Conversely, eccentric Achilles exercise protocols were found to increase the risk of future symptoms in the Achilles
Applications for Gymnastics For Reducing Risk
So from this research and my experiences, here is a list of possible (keyword) factors to consider. As this blog gets into the gymnastics community, I’ll be sure to update this with things I’ve gotten wrong, have been off the mark on, or maybe have an incorrect interpretation of.

-
Non Modifiable Factors
Before diving into things we can change, it’s important to recognize the things we maybe can’t. As was discussed, there may be a predisposition to Achilles issues due to the reduced blood supply in the watershed area of the tendon. Also, individual genetic differences in fibril size, tendon thickness, collagen make up, bone structure, and other factors are relevant. There is always the possibility of a clash between individual genetic make up, and the inherent fact that gymnastics is a jumping and landing sport with high risk. Every sport has its relevant inherent risk and more common injuries (baseball + shoulder injuries, boxing and concussion injuries, etc).
It’s also very important to highlight that the sport has just clearly gotten harder in the last 20 years, with bigger skills being done every year. The equipment has also evolved a ton, and we see much different engineering between types of floors/vaults/etc. I’m not going to dive into the engineering of floors for comparison, as I am absolutely not an expert in this area of mechanical engineering research. If there is someone reading this who is, please reach out to me with the latest research and I would be happy to include it here.
-
Pre – NCAA/Elite Training Factors
The most prominent finding from the literature I read is that tissue samples from both the Achilles that is torn, and also the contralateral Achilles that isn’t torn, appear to have pretty significant signs of degeneration. There are molecular and tissue level signals of a tendon that has suffered many cycles of repetitive microtrauma, with evidence of chronic inflammation and a lack of complete healing.
This wasn’t always the case, as the research was mixed, but there was a strong prominence of it. The take away is that it appears that tendons may be accumulating lots of damage either cumulatively or in a short window of time prior to the tendon tearing. It seems plausible that some of the bigger factors at the culture/training environment level need some serious consideration.
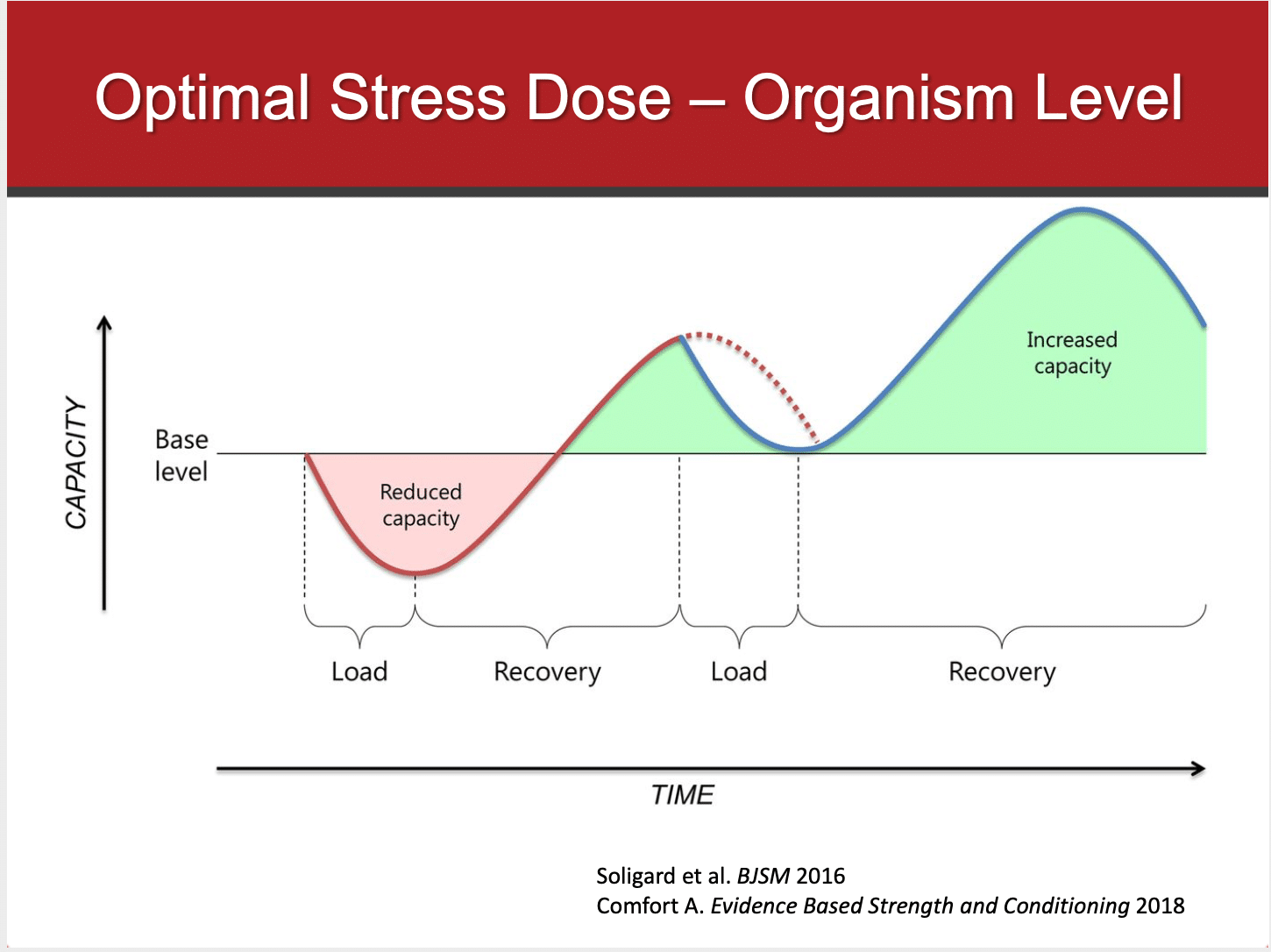
There are many factors that go into tendon health, and overall health for that matter. Tendons need an appropriate dose of overload stress to increase their capacity. But the key factor is that stress must be dosed appropriately, and followed by proper recovery time windows as well as proper recovery environments. Meaning that we not only need enough time between high loading bouts, but also the right amount of sleep, nutrition, hydration, etc to give the body what it needs to repair tissue. With this in mind, in terms of reducing risk I think we should be looking at
-
Year-Round Training
One of the most immediate concerns that pops into mind is that gymnasts continue to, for the most part, train all year long with minimal time off. The majority of younger gymnasts get 1-2 weeks off after competition season, and some time off for the holidays or vacations sparsely through the year. I’d confidently say the majority of gymnasts train 50 or so weeks per year starting from a young age. This new study from 2019 in JSMS reported a 2.62x increase in the odds of reporting a ‘gradual onset injury’ for athletes ages 10-13 who exceeded 8 months of training in a single sport.

As some significant research has suggested (read more here, here, and here) early specialization, and the year round training that usually comes with it, is of great concern. This goes for injury risk as well as overall athletic performance potential. It may be worth heavy consideration to impose an off-season for gymnastics. 2-4 full weeks off, along with 2 weeks of slow ramp up to high-intensity training may make a heavy impac. It may reduce the risk of injury at younger ages, but also to reduce cumulative damage over a career.
Many people would freak out at this saying there would be no time to get new skills and prepare for competition season. However, I think this is a bit far fetched. It also doesn’t have great solid scientific evidence behind it. There are plenty of JO, NCAA, and elite gymnasts who either voluntarily or involuntarily (due to injury) take 6+ months off and come back just fine.
For JO programs in the United States, maybe we need to have a conversation about encouraging a month off after the last competition. Maybe we also need to push back ‘summer’ training from June to September and have a longer preseason from October – January with a condensed competition season from February – May. This could still get 6-8 meets in, have States in early April, Regionals in late April, and Nationals in Mid May.
It’s much easier to say it than actually do it. I could be far off the mark, but just something to consider. I know coaches and parents might be happier with not having a massive 7-month grind of the competition season. As for that month when the gymnasts are off, gyms need income and coaches need paychecks. Tons of camps, clinics, staff education, planning, and yearly planning could fill that time.
Sure younger gymnasts need more time in the gym to learn skills and develop, but that’s a far cry from crazy hours and 50 weeks a year of gymnastics starting at age 8 or 9. One possible way to reduce risk this Achilles issues (and many other injuries) may be entertaining a longer preseason, with a shorter competition season, and not having back to back meet weekends. This may help gymnasts increase their capacity for loading prior to the tough competition season. It would also allow more time between high loading to repair tissue, and would reduce the toll a competition takes on a young athlete who is still developing (if safely implemented.
-
Early Specialization
Closely related to the concern for year-round training is the concern for early specialization. Either directly or as a cultural undertone, gymnasts are encouraged to do only gymnastics from a young age. The defense for this is that the sport is so unique and demanding, they need to ‘get ahead’. This is a big concern, as the lack of sport variability tends to produce excessive stress on certain areas of the body and creates the risk of burnout.
The same 2019 JSMS study above highlighted a 1.6x increase in odds of reporting ‘gradual onset injury’ when the number of hours in a single organized sport exceeded the age of the athlete, in a group of 10-13 year olds. (i.e. a 12 year old training 15 hours per week in a single sport). It’s interesting to note that in another study of athletes ages 14-19, a 4.41x increased odds existed for reporting a sports-related injury for those that trained significantly less hours per week compared to their age (a 15 year old training 10 hours per week in a single sport).
This is in line with a 2017 paper from The American Journal of Sports Medicine looking at 2011 athletes. They reported that athletes who were in a primary sport > 8 months per year were more likely to report an upper extremity overuse injury (OR = 1.68) or lower extremity overuse injury (OR = 1.66). Athletes who participated in their primary sport more hours than their age were more likely to report an injury (OR = 1.34). I think both of these papers really connected the dots for me on Achilles issues, among many other common gymnastics issues like lower back stress fractures, elbow OCD, and Gymnast Wrist. (More research from this area on that here and here)
The take away here is that maybe when younger and at risk overuse injury around ages 8-13, we need to respect age to training hour ratios more carefully. But, as puberty passes and athletes take on bigger goals, we need to encourage slightly higher age to training hour ratios to build physical fitness and resileincy against injury. This is in line with workload research as I’ll discuss below, as we want to safely build to high workloads to build a buffer against injury risk and increase performance.

In baseball, the concern is for shoulder or elbow issues. In soccer, the concern is for hamstring and knee issues. In gymnastics, one concern is for ankle impact injuries that stress the joint and Achilles. If gymnasts were able to delay specialization, the hope would be that a variety of sports could help reduce the risk of focal overload to certain areas like the ankle and Achilles. This is especially relevant during at risk time periods like pre-puberty and puberty.
If you total up the number of impacts from tumbling, landing, and running, gymnasts likely take 1000s of impact per month as kids. There is no research connecting this to causing Achilles injury in gymnasts, but it’s been suggested as a correlate risk factor for youth sport. Yes gymnastics is unique and if you have high-level goals specialization is inevitable. But delaying single sport specialization until at least 12/13 years old (most other sports are 15) might be one way to reduce the risk significant injury at that age and later in ones career.
I will say that the ability to reach success and overcome these new changes would require massive work, patience, and time from the gymnasts, coaches, medical providers, and patients. It’s no easy feat, but it can be done with effort and collaboration.
-
The Need For Traditional/Mixed Strength and Conditioning With External Weight Lifting in Gymnastics
At this point, it’s very important to highlight how under training is just as concerning as overtraining. Acute spikes in training load have been raised as a concern for injury risk (research here. here, here and here). This is important to consider, as the Achilles tendon research above discussed repetitive microtrauma creating degeneration in the samples from Achilles tendons that are ruptured, and how this degeneration can come without symptoms of pain.
Safely building to a high chronic workload helps build a buffer against injury risk. This is because the athlete becomes more resilient and robust to handle the demands of competition season. We want gymnasts to train hard and increase their fitness, both for health and skill progression, but we have to do it safely. This is where traditional strength and conditioning can play a role. Despite mountains of evidence in support of the benefits of external weight lifting for youth athletes (find some here, here, and here), gymnastics still continues to be resistant to implementing it.

Adopting formal external weight lifting for gymnasts serves as an intersection for being able to increase capacity, while also not depend only on gymnastics specific training. Keep in mind, it should serve as one piece to a gymnasts physical preperation work, and traditional gymnastics strength is crucial to perform each day.
The concerns for gymnasts getting ‘bulky’, getting hurt, or losing their flexibility can be put aside when properly implemented, as I wrote about in this article here. It has been demonstrated as safe for young athletes when properly implemented, with proper progression, and good technique. The key here is that strength coaches need to better understand the sport of gymnastics, and gymnastics coaches need to be open to the idea that there are professionals who do this as an entire career and can help our athletes.
-
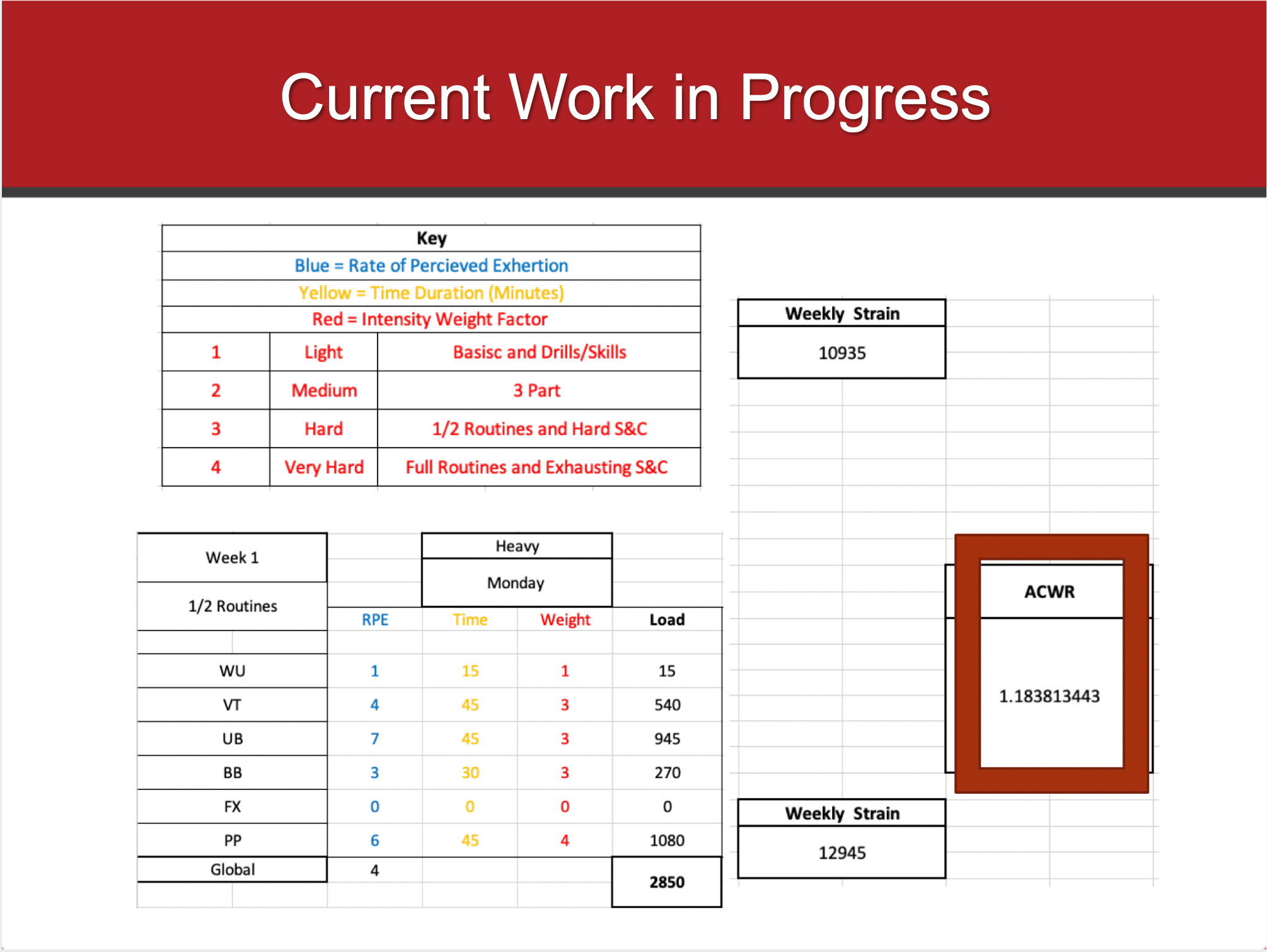
The Need For Structured Periodization Use
This goes directly with the points above. Periodization is the science of rotating light, medium, heavy, and off training days to help the athlete safely accept and adapt to training loads. Despite a significant amount of research in this area displaying benefits (find more here, here, and here), the gymnastics culture still has largely failed to implement it. There are some gyms that implement this principle very well, and fully understand it. But as a whole, I think it’s not considered or implemented fully across all of gymnastics.
I do think there is a large piece of this that comes from the global education side of things. There is a huge lack of information for coaches who want to learn about proper periodization and programming strategies. Even more, many are on board but don’t have direction on ways to practically implement periodization research into daily gymnastics practice. Regardless of this, we must adopt formal principles if we want to see the benefits.
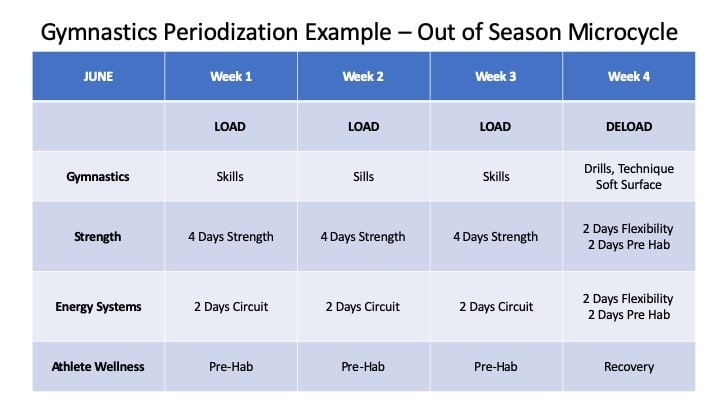
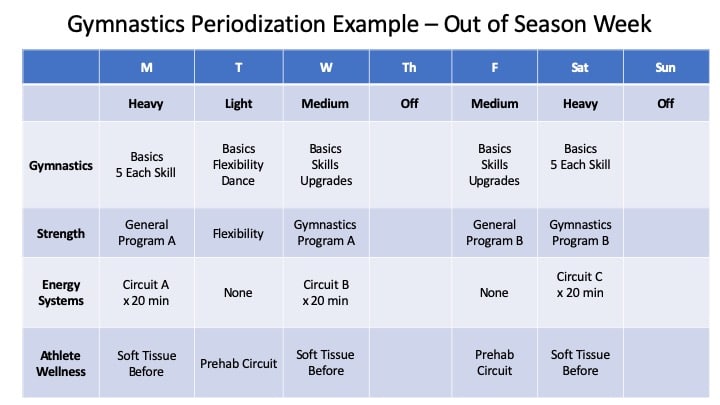
If we want to make a dent in the risk and rates of Achilles tendon injuries, I think we really need to educate coaches and gymnasts in the pre NCAA levels on the use and implementation of periodization. Gymnasts need more optimal rotations of light, medium, and heavy days. We can’t just go super hard multiple days per week and then hope no one gets hurt. Also, we can’t be scared of all injuries and not train on hard surfaces or go all out everyone once and a while. Periodization helps guide the balance. This leads to another point about workload monitoring.
-
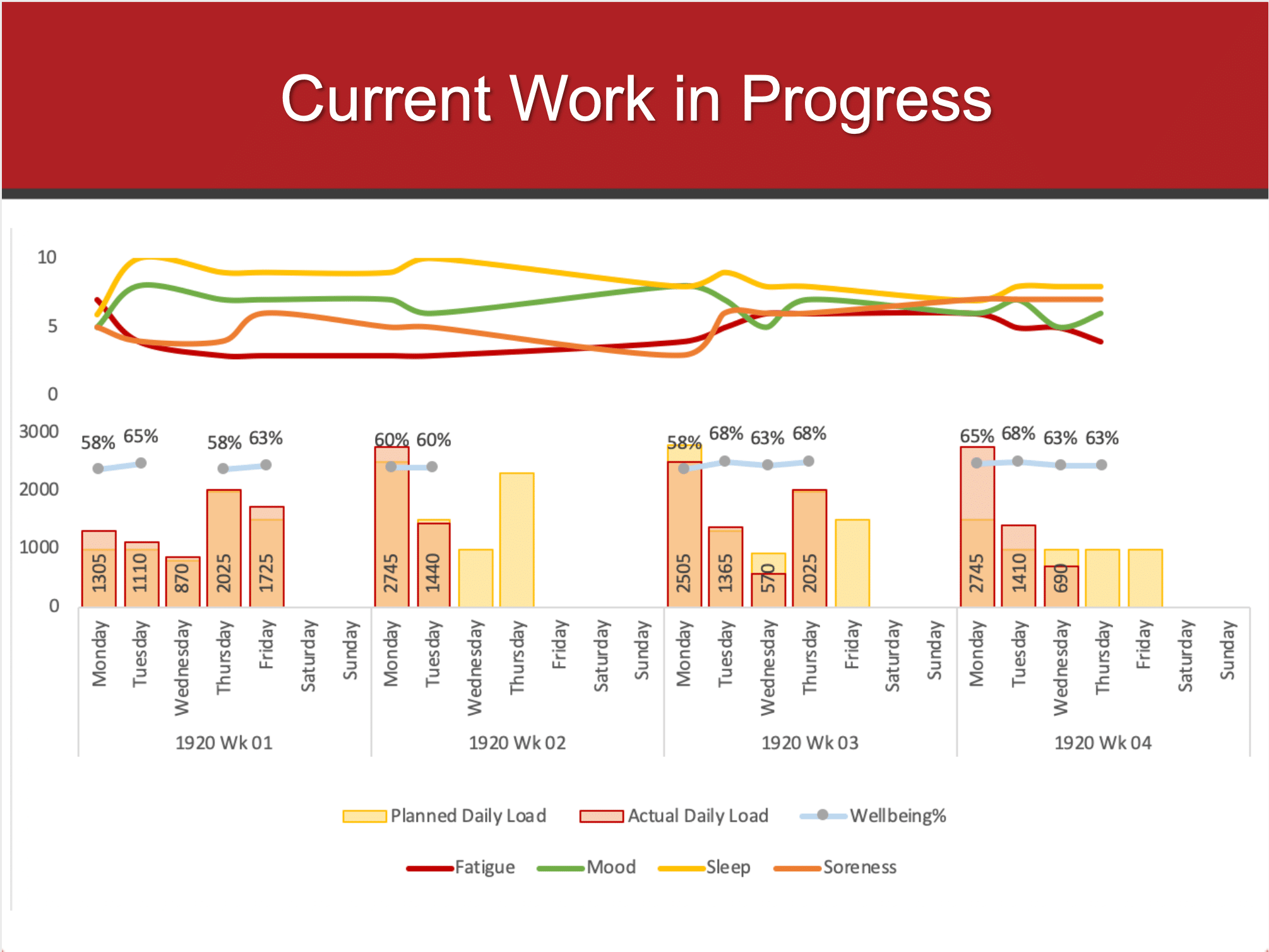
The Need For Workload Monitoring, Prescription Tools, and Guidelines
As noted, we now have a good amount of literature to highlight the concern for sudden spikes in workloads, as well as not safely reaching a high chronic workload, in relation to increasing the risk of injury (research here, here, here, and here related to elite university athletes). This matters for Achilles issues because if we don’t know how much we are changing workload day to day, week to week, and planning these things out, we might get in hot water fast.
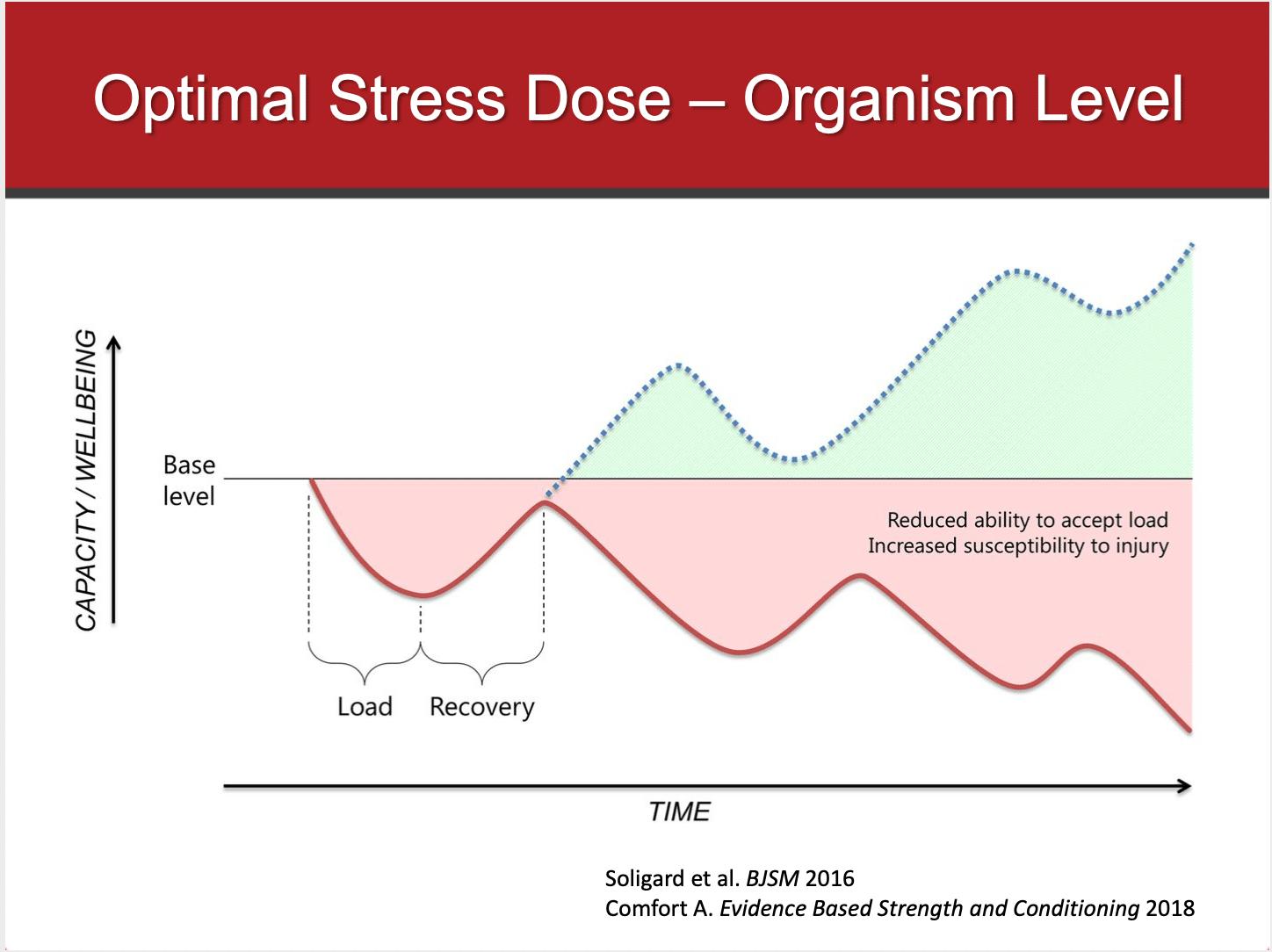
Tim Gabbett’s lastest paper brings a fantastic view on this, discussing the need to identify the “floor” (baseline of capacity at season start) the “ceiling” (the highest amount of workload a gymnast needs to perform) and the time to get athletes from the floor to the ceiling.
Gymnastics needs better systems to measure workload both globally for overall fitness/fatigue, but also locally for the specific measurements like lower body impacts, back hyper extensions, and shoulder/wrist specific impacts. We also need to use tools to understand the most demanding periods of the competition season and planning tools to help map out a safe progression to high chronic training loads that are suggested to buffer injury. These are crucial to make a change in big injuries like Achilles tendon tears.
-
The Need For Discipline Around Proper Technique and Performance of High-Risk Skills
This is crucial. I can’t tell you how many times I did skills I was not fully ready for, or didn’t have the best technique for. This matters for the Achilles stress during take offs, and also landings.
I’ve had many questionable landings where I destroyed my ankles. The worst part is that my stubborn nature and the cultural undertone was to just walk it off (or limp it off) and either try again or give it a day before trying again. It doesn’t happen everywhere, but it’s still common. This is not healthy, and likely has massive negative ramification for tendon health as well as bone and other areas over time. The best training practices won’t go far if egos and a lack of patience are on the table.
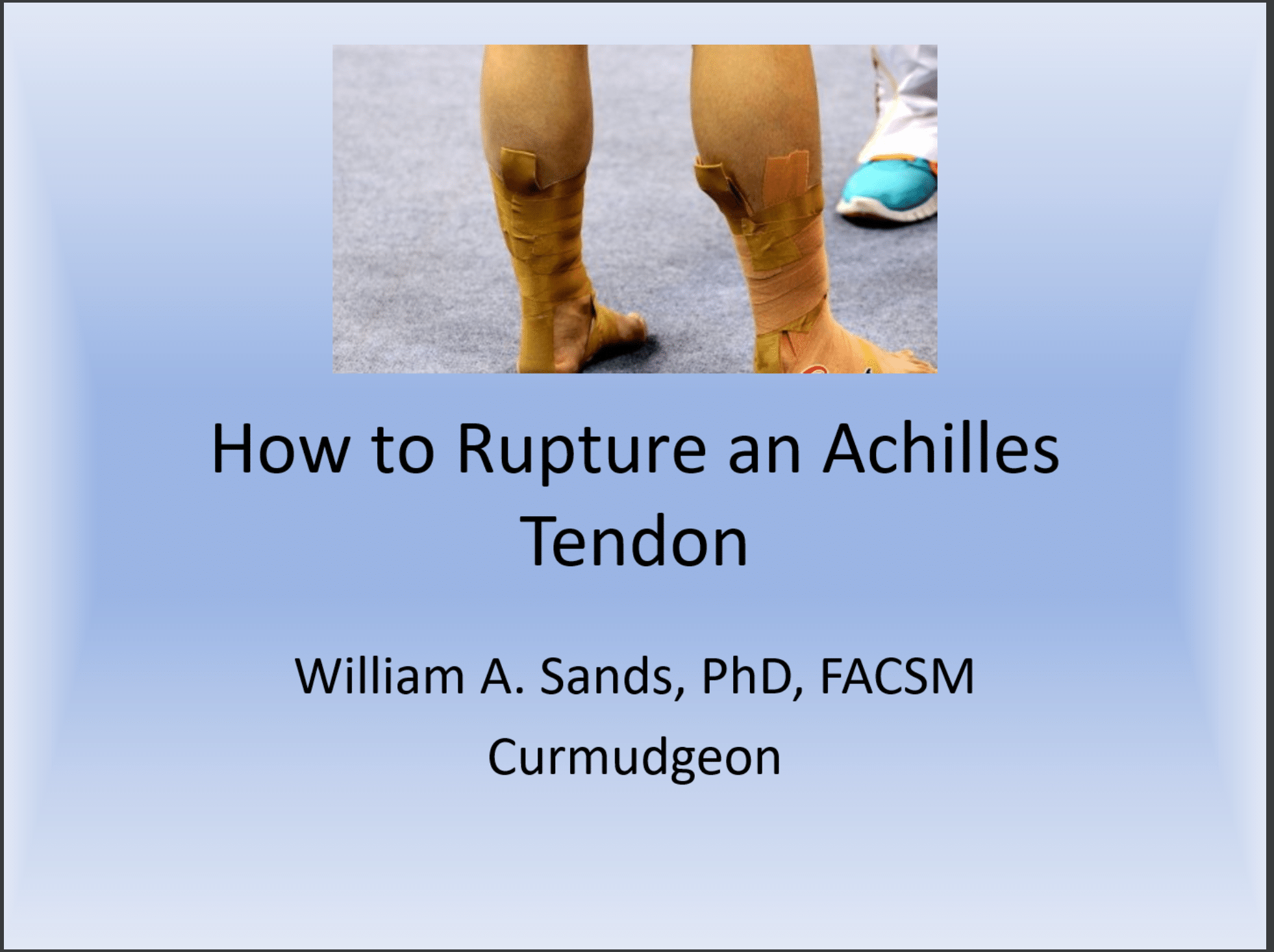
Closely related, there is definitely evidence from experts like Dr. Bill Sands to suggest that different types of tumbling make a big impact on the risk of Achilles tears. Concerns for very steep tumbling angles and a lack of stiffness on the floor might cause ‘knee reversal’ during tumbling or vaulting that has to be considered.
An example of this is shown below, where rather than being stiff on the board this athlete is getting a notable knee bend that is not as ideal. The interaction between the tumbling technique, knee bending, and springs in a floor/board are definitely factors we need to consider.

*2/25/2020 UPDATE* – After publishing this article, Dr. Bill Sands reached out to me directly and generously offered some more ideas based on the points above. He was kind enough to offer me a great slide show he made in the 2000’s called “How to Tear and Achilles” and has loads of amazing information/videos about tumbling technique and the equipment. 100% credit goes to Dr. Sands. You can find it here,
Click HERE to view the full slideshow for free.
This speaks to the need for everyone to be more disciplined about both optimal tumbling techniques and knowing when is or is not the right time to do new skills. This means learning this, as well as implementing it. Sure gymnasts can be stubborn or not want to listen, but it’s up to us to explain why it’s so important and be the gatekeepers for progression to more advanced skills only when things look good technically, and the athletes are physically/mentally prepared.
Gymnasts need to respect this, as well as coaches and parents. I have seen 100s of young gymnasts do skills with very concerning technique, or do skills they are not ready for at practice or meets, masked behind a terrible defense of ‘just going for it’ or courage. This needs to stop at the younger levels. Globally, I’m not sure if this is the only factor that causes rupture. We dont’ have the evidence to look at every gymnast, including high-level NCAA/Elite, who have torn their Achilles to map the data.
The take away is that proper technique, foundation, and progression is key for safety. Even if it appears that someone doesn’t get hurt from it, no pain doesn’t always mean no problem. Don’t let immediate gratification get in the way of long term health. Not flipping a vault or doing a tumbling pass may upset someone who is nervous about social judgment from their peers, but it’s better than being out for a season with a huge injury. Take the time to fully develop technique, progress drills, and get physically fit enough to do hard skills. To gymnasts and parents, patience, persistence, and work are the foundation.
-
Local Ankle Mobility and Strength Care
I intentionally put this point later in the list, as I think often times people are quick to assume or jump to conclusions about ankle flexibility and localized strength. Sure, excessively stiff ankles and very limited calf flexibility can be an issue for the risk of Achilles tears. But, the best ankle flexibility and strength program will fall very fall short if the factors above aren’t considered.
Very limited soft tissue and ankle flexibility are suggested by some a risk factor for rupture. Gymnastics demands extreme ankle mobility, especially during vault and floor where many ruptures are seen. If repetitive soft tissue damage occurs through training without and recovery work, a problem may exist with overload. That being said, there really isn’t a consensus on the ‘ideal’ amount of stiffness. An appropriate amount of stiffness is needed for power and tuning the equipment, and some of the best gymnasts in the world have stiffness in their calves. Again is the paradox between risk and sport requirements.

This also goes for local ankle strength. It’s critically important that the gastrocnemius and soleus muscles are appropriately strengthened. However, people are wrongly looking for the ‘best pre hab exercises’ without admitting the bigger technique, global physical preperation, and workload issues above. A huge amount of loading goes through the calf complex, so more muscular support and conditioning of the tendons must occur. But it’s a small piece of the puzzle. Implementing things like seated weighted calf raises, dumbell tiptoe walks, and other loading drills does come to mind.
-
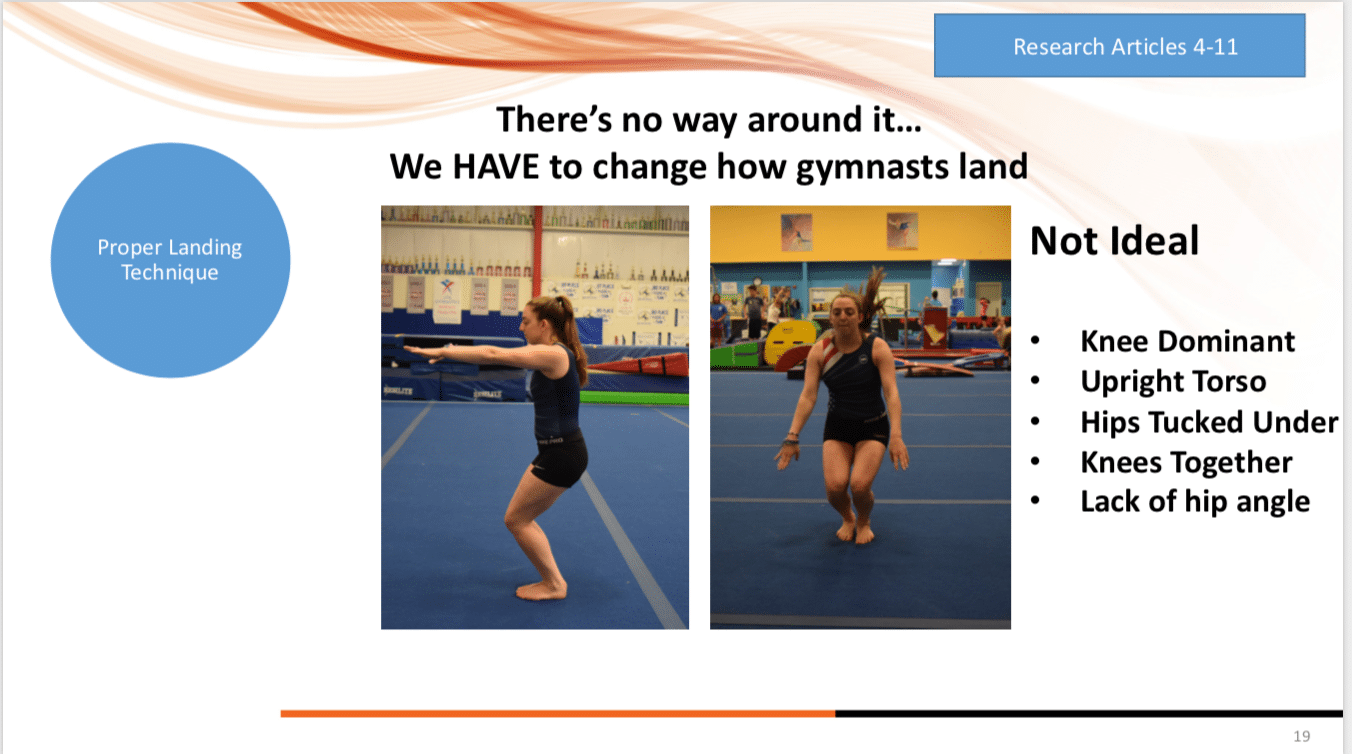
Proper Landing Techniques
This one has made some significant progress in the last few years, and honestly applies to both pre and during NCAA training. After a few years of concern, I wrote this article “Why Gymnasts Must Change How They Land” (click here to read) which covers many of the foundational concepts.Many more coaches, gymnasts, and judges are realizing the very dangerous risks of landing in a less biomechanically safe position of the feet together, torso upright, and ‘knee dominant’ landing.This is opposed to what multiple research studies suggest (more here, here, here, here, here, and here) is a safer landing of the feet hip-width apart, the torso parallel to the shin angle, 30 degrees of hip angle, and more of a ‘hip dominant’ landing. The more hip dominant landing helps shift forces away from the knee joint, as well as the ankle/Achilles, to the musculature of the entire lower body for better force dissipation.Obviously more of the issues with Achilles tears are during takeoff for tumbling/Vaulting, but there have been issues with short landings. The repetitive microtrauma that comes on the Achilles tendon and the ankle joint also factors into the cumulative impact volume mentioned earlier. Being able to only do skills when a gymnast is physically, mentally, and technically ready for the landing is key. Gymnasts must also be taught the difference between proper gymnastic specific ‘bounding’ form and proper squat form for landings. Both are needed to perform well and optimally protect the athlete.
-
The Need for Formalized Education For Coaches
It is definitely clear that there is a void in most educational systems, but certainly in the United States, for new and existing coaches. It is a bit frightening that there is no mandatory, systematic education system required to become a coach other than some basic safety certifications. The lack of comprehensive education about basic anatomy, physiology, injury mechanisms, technique, strength, conditioning, and how to safely develop athletes raises large concerns. There are some foundational guides around the world, especially at the elite international levels, but we still need much more work to be done for optimizing this.
For existing coaches, there needs to be some guide for ongoing education. This is partly the best practices of gymnastics training evolve rapidly. I laught at some of the things I was doing 10 years as a coach. Also, scientific information changes at a blistering pace. Coaches, parents, gymnasts, and medical providers need to be aware of this, spend time learning, and then adapt that to their training.
-
The Need for Better Medical Understanding of Gymnastics
On the other side of the fence, I think there are many times we drop the ball on the medical side. Most medical doctors and rehabilitation specialists don’t understand the specific demands of gymnastics, even in the sports and orthopedic world. If there aren’t medical providers who understand the sport and can fully rehabilitate gymnasts with solid strength and conditioning principles, we may leave them at risk for re-injury or progression of injury. This wraps in the issues with insurance and medical care as a whole, but that is a much bigger discussion.
-
Accountability For Coaches/Parents Who Push Too Hard, Too Young, and Too Soon
This is more of a moral piece, but also comes with the need for checks and balances. The majority of coaches and parents just want to see gymnasts do well, maximize their potential, and stay safe in the process. However, we can’t ignore the reality that there still exist coaches who have large egos, questionable motives, and inappropriate methods for training young gymnasts. These coaches need to be held accountable for pushing young gymnasts too hard, and too soon.
It falls on the global organization level to publish guidelines and policies about the number of hours gymnasts should train at certain ages, the ranges of training volume that is concerning, what training should be comprised of, and if the competitive levels that young gymnasts are allowed to compete at is optimal. Much of the impact volume and specifically Achilles/knee issues may be combatted if we address these problems. “Training through” Severs and Achilles tendon issues when young is very dangerous.
-
The Need For Gymnasts/Parents To Care For Themselves Outside The Gym
We can’t count out the fact that gymnasts and parents need to be maximizing recovery outside the gym. Many of the tendon issues, as well as bone issues, we see in the younger levels have a massive factor of proper recovery techniques.
Gymnasts not only need the appropriate time between heavy loading bouts, they also need proper quality/quantity of sleep, proper nutrition, adequate hydration, and outside the gym stress management. Tendons that become degenerative and break down, and then go on to possibly rupture when older, could be combatted with better recovery practices. These factors also greatly impact the athlete’s mental state for the ability to have solid technique during training sessions.
This also speaks to the need for parents to not put excessive pressure on their young kids just for social media posts or a sense of pride. Gymnastics is a marathon, not a sprint, and the worst thing parents can do is go crazy with extra hours and private lessons. Putting in work is one thing, getting run into the ground is another.
-
-
NCAA / Elite Training Factors
Even though there are many factors for improvement at the pre-college level, there are many things that need consideration at the NCAA level. Most of these come down to conversations about NCAA season workload ratios, the athletes capacity both starting college and at the start of preseasons, and discussions about the format of college competition seasons.
-
Responsibility To Stop Early College Recruiting
This concept directly impacts many of the factors above in the pre NCAA section. Plain and simple, early recruiting still continues to be a huge problem that needs much more strict rules and accountability. I’ve discussed this on the podcast with Tom Farden of Utah Gymnastics, Olympic Coach Tom Meadows of Cyprus Academy, and Bridget Soan of Florida.
Even if it is not intended, the pressure of early college recruiting causes coaches and gymnasts to want to do hard skills at a young age. It is usually when they are in prime vulnerability during puberty. Club coaches, parents, and gymnasts often get wrapped up in the desire to ‘get noticed’ by colleges sometimes as early as in middle school. This is madness.
We really need to have a conversation about the high force skills young gymnasts are doing while going through puberty. We need to think hard on if that’s the optimal situation for both physical and mental health. I’m all for helping young talented gymnasts develop, and for making sure we can maximize someone’s potential if they have big goals. But that doesnt mean competing all the hardest skills someone can do all the time. If 9-year-olds are flipping Yurhcenko’s and doing fulls on hard surfaces, then at 13-15 they are doing Yurchenko fulls and flipping double backs on hard surfaces, that is a lot of workload coming on the Achilles.
It’s hard to comprehend, but introducing high impact skills that young could mean 1000s and 1000s of more impacts on the ankle and Achilles in the years prior to college. Not to mention any short landings, mishaps with one legged landings, or accidents, which are also inevitable even with great stategies in place.
This speaks to a larger issues. The NCAA Goals study showed that incoming freshman gymnasts had the highest rates of ‘significant injury’ prior to college, indicating large injuries or surgeries. This could be a big factor of setting up an Achilles tendon rupture as in the college the meet season is very dense compared to the JO season. Many weekens are back ot back weekends, with some having even less time intervals between them.
Not to mention collegiate gymnasts are often performing higher power skills during these high density competition seasons, and are fully mature athletes. This is up to all of the coaches in the NCAA, as well as JO coaches, and the NCAA as an organization, to put their foot down on. Parents also have a role, as well as the gymnasts, to ease off the pressure when young.
-
Maintenance of Off-Season Workloads
I think this is a big one more so for the gymnasts themselves in college. As mentioned above, it’s important to have off time and recovery periods after season finishes. College gymnasts need that time for physical and mental recovery, not to mention school.
But, in the months of June through August, gymnasts need to be putting in the work to maintain their capacity and fitness. This also goes for maintaining workloads during injury, as this Australian Institue of Sport paper showed reduced time to return to sport after injury based on the amount of workload maintained (safely)

As mentioned with Tim Gabbett’s articles, not keeping up workloads may cause the ‘floor’ to be much lower upon return to pre season, which Tim indicates as the ‘basement’. It then becomes a time crunch to get fit enough and prepared for season once back at school.
If this is not managed, the spikes in workload may come too soon, and set someone up for Achilles issues. It may be slow degeneration that primes the tendon for bigger issues like noted in the studies above. It also could just be less capacity of the body to handle the long grind of the competitive season that elevates injury risk, with limited time for recovery and full tissue healing.
-
Better Workload Systems, Monitoring, and Research
We really don’t have any objective ideas about what a normal daily, weekly, or season workload looks like for a college gymnast. There are some ways to look at internal and external training load, but to my knoweldge none have been super specific to gymnastics.
How can we help gymnasts prepare for the long grind of a season, Regionals, and Nationals if we don’t even know how hard they are? We need much more research and funding to help explore global and gymnastics specific monitoring tools for NCAA gymnastics. In an ideal world, we would be able to build a valid and easy to implement system that looks at global workloads (wellness, training loads) as well as sport specific loads (ankle impacts, back hyper extensions, shoulder stressors). This is an area of research I’m actively invovled in.
Closely realted to this, we still don’t have great biomechanical data for the hardest skills or situations in gymnastics. Floor tumbling has demonstrated 14.9x bodyweight forces, with the Achilles around 18x recorded and the tibiotalar joint at 23x bodyweight (that data in these books here and here). But, that is definitely not the highest demand. Much harder E tumbling passes, steep tumbling take-offs, landing short, or incompleted twists that put all the force on one leg, are likely much higher demands on the Achilles.
If we want to better understand how much capacity is needed or meet season, how to plan for the preseason, and if we need to make changes to the competitive season, we need to understand what the current state of workload is on the average NCAA athlete. If we really want to understand Achilles ruptures, we need better data on the loading rates and biomechanics of the skills NCAA gymnasts are performing.
There is an abundance of information in other sports to measure and track workloads, then apply concepts like acute to chronic workload ratios or specific tissue loading rates (UCL injuries in baseball). We need to keep developing and testing different gymnastics workload paradigms, and look for patterns.
-
Correction of Tumbling/Vaulting Technique
This kind of goes without saying from the above section, but it’s crucial that incoming NCAA gymnasts correct any technical issues in their tumbling mechanics. As mentioned, a nonoptimal technique of ‘knee reversal’ from a lack of stiffness on the springs, as well as super steep take-off angles, might be a significant risk factor for Achilles injury. When an incoming NCAA Freshman joins a college competition format that has a much denser competitive season, who is now fully mature and more powerful, and may be specializing in only a few events, that could be a very high-risk situation.
-
Diversity of Event Profile
We do need a global perspective for training workload and athlete wellness. We also need a more narrow perspective about event-specific workload, in this case the number of impacts/landings. I think this is even more important in the NCAA as many gymnasts move to specialize in events, versus doing all around in younger years.
If a gymnast drops uneven bars or beam, that may put significantly more workload on the Achilles tendon and lower body. After years of loading, and possible degenerative tendon states mentioned above, it may be setting up the perfect storm for the risk of an Achilles rupture.
Other factors with this include the ability to rotate the focus of events. It’s inevitable that gymnasts will do heavy impacts, and we need to build their capacity for this safely to help develop fitness and resilience against injury in season. I’m not saying or suggesting we shouldn’t do high force loading that the sport requires.
That being said, there are plenty of ways to work these events over the course of the week to build capacity. This can also be developed with more integrated and gymnastics specific strength and conditioning in the off season/preseason which will be touched on below.
This also connects to emotional intellegence of coaches to read the athlete and communicate about when to push or pull back. As this 2016 suggested, high academic stress have been linked to elevated injury risk and illness in the NCAA football players.
-
Longer Pre-Season Timelines
Going back to the workload concept, one of the suggested ways to help reduce the risk of injury is to increase the overall capacity. With changes made to the ‘floor’ coming into a season with higher fitness levels, a longer preseason timeline may also help build resistance to injury. The longer the time interval, the most we can safely build to a high chronic workload prior to the competition season. Tim calls this reaching the “Penthouse” of capacity; an above expectation level of fitness/readiness before competition season.
Most NCAA programs are already doing a great job with their pre season timelines, and there isn’t an infinite amount of weeks to prepare. But, being able to push the envelope safely and train hard in the preseason is key. Again, this goes back to why we need workload systems to see data behind these weekly loading cycles, and we can’t just guess.
It’s easy to lose sight of how far away the competition season is, but it always creeps up much faster than expected. This is a situation where spikes in training volume, especially for floor and vault routines, may occur with elevated risk. It may also lead to a lower overall chronic workload, which means athletes have a reduced fitness level going into the long meet season and increased risk of injury / under performance.
-
Changes to Competitive Season Structure
Even though there is a large range in when Achille tears occur, there is a huge number happening during the competitive season. As noted, 4 weeks into 2020 there have been 20 tears. Each year continues to show alarming rates of more athletes with ruptures that are season-ending, sometimes career-ending, and definitely life-altering.
Along with considering off-season capacity for the “floor” of workloads, and building in the preseason to the “ceiling” of workloads, the actual competition season then becomes an area to discuss. One thought about repetitive microtrauma to the Achilles tendon that might predispose risk is the time interval between high impact loading instances. It could be that the shorter, denser layout of NCAA season compared to younger JO years is an issue.
I’m not sure if this would be a way to mitigate risk and rates of Achilles tears, but conversations about shortening the competitive season might be warranted. This would allow for increased preseason to build capacity, and reduced high impact loading rate (if implemnted correctly). Other ideas are not having as many back to back meet weekends or competitions so close in proximity to allow tendon recovery. Again, I’m sure college coaches already factor this in and I’m just not aware of it. I also don’t coach college, so we need many more voices but my own here.
This also gets tough with the new format with Regionals and NCAA being multi day. NCAA Coaches are (rightfully so) training to mimic these demands. The ripple effect of this 2019 change is still shaking out as years roll on. It’s hard to tell how these changes would all impact injury rates with shorter seasons, or maybe just more time between meets/high impacts. There is also the idea of rotate people into floor/vault line ups, which many already do. But, not every team has infinite depth.
-
Better S&C Practices to Build Capacity
This is also a shared responsibility, but NCAA coaches, S&C coaches, and medical providers need to be on the same page about screening and pre-season physical preparation. Just blanket applying a general S&C program to gymnasts definitely will be problematic. I’m the first one to say that the wrong S&C program applied to college gymnasts can make things much worse, not better. In addition to this, within a gymnastics team, there is so much individuality that needs to occur due to backgrounds, injury history, event specialization, and so on.
It may not be that specific eccentric exercise protocols are needed for the Achilles during S&C, but more so just a general well-designed program to help build capacity specific to gymnastics. This refers to both overall aerobic fitness (as that has been shown to be a moderator of injury risk) and also gymnastics specific strength/power work to complement work done in the gymnastics gym during preseason. We also need gymnasts to buy in to follow the plan fully. Lots of moving parts here. I always suggest that immediately upon return back to school, people start with full gymnastics movement screens (find mine for free here) and communication.
This can then be used to build strength and conditioning programs that are specific to the sport of gymnastics, and specific to the gymnasts themselves. It’s also worth noting that this long 12 week window is a great time to build the tolerance to impact and conditioning tendons, moving from low, to medium, to high impact plyometrics. This must be carefully balanced with the gymnastics specific plyometrics, but this can theoretically help build the Achille’s capacity to accept high load.
-
Screening Tools for At-Risk Athletes –
This is building off the global movement screens above. I think that global movement screens are huge for all NCAA gymnasts, particularly the incoming freshmen who may carry with them lots of accumulated issues. Many gymnasts don’t want to speak up about their injuries or past issues, in fear of not training/competing. We will always face this, but it has to be communicated that for the best of the overall health of the athlete and team performance, that openly addressing injury issues is the best option.
Past this, there may be more focal screens that might help out with Achilles issues outside of just identifying movement issues or prior Achilles injury. The research above outlined how neovasularization and hypoechogenicity might be an early risk factors to look at. That’s along the working theory of progressive degeneration leading to increased risk of Rupture, which is still unclear in gymnasts. Looking for signs of chronic inflammation or tissue degradation/disorganization may be something to consider. I’m not an expert in this field, and I know there are financial/time implications of this, but maybe there are easier to use technologies out there that can be utilized.
-
Conclusion
So, this was clearly a beast of a topic to cover. But, I wanted to make sure I was thorough to display the complexity of this issue. I also wanted to try and touch upon a variety of factors that may go into the high rates of Achilles tears, so we had a lot of ideas for possible ways to reduce risk.
Hopefully, the great research that has been done, and also articles like this can help spark conversations. For all these reasons, there definitely has to be some more things done to help combat the high rates we are seeing. Work has to be done at the younger levels, and at the NCAA/elite levels. These issues have far reaching impac beyond just Achilles tears, Back fractures, shoulder issues, wrist issues, and many other overuse injuries fall under this umbrella. Remember that these are just my interpretations of the research, and my opinions about what is going on.
I’m looking forward to Part 2 of this blog, where I sit down with a leading tendon expert in this field. She will shed some more light on the issue, and also help set anything straight I said here that might be off the mark. For now, hope you enjoyed reading. Have a great week,
– Dave
Dr. Dave Tilley DPT, SCS, CSCS
CEO/Founder of SHIFT Movement Science
References
- Chan JJ., et al. Epidemiology of Achilles tendon injuries in collegiate level athletes in the United States. Int Orthop. 2020 Mar;44(3):585-594. doi: 10.1007/s00264-019-04471-2. Epub 2020 Jan 6.
- Elengard T., Karlsson J., Silbernagel KG. Aspects of treatment for posterior heel pain in young athletes. Open Acces Journal of Sports Medicine. 2010:1 233-232
- Arnold A., et al. Overuse Physeal Injuries in Youth Athletes: Risk Factors, Prevention, and Treatmenet Strategies. Sports Health.2017; 9(2)
- Dederer KM., Tennant JN. Anatomical and Functional Considerations in Achilles Tendon Lesions. Foot Ankle Clin N Am 24 2019: 371 – 385
- Winnicki K., et al. Functional Anatomy, Histology, and Biomechanics of the human Achilles Tendon – a comprehensive review. Annals of Anatomy 2020
- Dakin SG., Newton J., Martinez FQ, et al. Chronic inflammation is a feature of Achilles tendinopathy and rupture. Br J Sports Med. 2017; 52 359: – 367.
- Li Q., Zhang Qi., Cai Y., et al. Patients with Achilles Tendon Rupture Have A Degenerated Contralateral Achilles Tendon: An Elastography Study. BioMed Research International. 2018
- Schulz FK., et al. Different Achilles Tendon Pathologies Sow Distinct Histological and Molecular Characteristics. Int. J. Mol Sci. 2018; (19) 404.
- Splittgerber LE., Ihm JM. Significance of Asymptomatic Tendon Pathology in Athletes. Current Sports Medicine Reports. 2019; 18(6)
- McGowan J., Whatman C., Wlaters S. The associations of early specialization and sport volume with musculoskeletal injury in New Zealand children. JSAMS. 2020; 23(2): 139-144
- Jayanthi N., et al. Sport Specialization in Young Athletes: Evidence Based Recommendatyions. Sports Health. 2012; 5(3): 251 – 257
- Myer DG., et al. Sport Specialization, Part 1: Does Early Sport Specialization Increase Negative Outcomes and Reduce the Opportunity for Success in Young Athletes? Sports Health. 2015; 7(5): 437 – 442
- Meyer GD., et al. Sport Specialization Part II: Alternative Solutions to Early Sport Specialization in Youth Athletes. Sports Health. 2015; 8(1): 65 – 73
- Post EG., et al. The Association of Sport Specialization and Training Volume with Injury History in Youth Athletes. AJSM. 2017; 45(6):1405 – 1412
- Jayanthi NA., et al. Health Consequences of Youth Sport Specialization. Journal of Athletic Training. 2019; 54(10) 1040 -1049
- Bell DR., et al. Sport Specialization and Risk of Overuse Injuries: A Systematic Review with Meta-Analysis. Pediatrics. 2018; 142(3)
- Gabbet TJ. How Much? How Fast? How Soon? Three Simple Concepts for Progressing Training Loads to Minimize Injury Risk and Enhance Performance. Journal of Orthopaedic & Sports Physical Therapy. 2019; 0:1–9
- Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med 2016;50: 273–280.
- Soligard T., et al. How Much is Too Much (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016 Sept;50(17):1030-41
- Schwellnus M., et al. How Much is Too Much (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br J Sports Med. 2016 Sept;50(17):1043-42
- Faigenbaum AD., et al. Youth Resistance Training: Updated Position Statement Paper from The National Strength and Conditioning Association. JSCR. 2009; 23 (Supplement 5) S60-S79Danhab KS, McCambridge TM., et al. Strength Training in Children and Adolescents: Raising the Bar for Young Athletes? Sports Health. 2009 1(3): 223 – 226
- Granacher U., et al. Effects of Resistance Training in Youth Athletes on Muscular Fitness and Athletic Performance: A Conceptual Model for Long Term Athletic Development. Fronteirs in Physiology. 2016; 7(164)Evans JW., Periodized Resistance Training for Enhancing Skelatal Muscle Hypertrophy and Strength: A Mini Review. Fronteirs in Physiology. 2019; 10(13)
- Lorenz D., Morrison S. Current Concepts in Periodization of Strength and Conditioning for The Sports Physical Therapist. ISJPT. 2015; 10(6): 724 – 747
- Hartmann H., et al. Short-term Periodization Models; Effects on Strength and Speed-strength Performance. Sports Med. 2015; 45(10):1373-86
- Bourdon PC., et al. Monitoring Athletes Training Loads: Consensus Statement. Int J Sports Physiol Perform. 2017. 12(Suppl 2): S2161-S2170
- Hamlin MJ., et al. Monitoring Training Load and Perceived Stress in Youth Elite University Athletes. Frontiers in Physiology. 2019. 10(34).
- Ardern et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Br J Sports Med. 2018; 52:422-438
- Smith HC., et al. Risk Factors for Anterior Cruciate Ligament Injury: A Review of the Literature.- Part 1: Neuromuscular and Anatomic Risk.
- Smith HC., et al. Risk Factors for Anterior Cruciate Ligament Injury: A Review of the Literature.- Part 2: Hormonal, Genetic, Cognitive Function, Previous Injury, and Extrinsic Risk Factors.Pietosimone LS., et al. Landing Biomechanics, But Not Physical Activity, Differ in Young male Athletes With and Without Patellar Tendinopathy. J Orthop Sports Phys Ther. 2020; 6:1-30
- Launat F. Sports related overuse injuries in children. Orthop Traumatol Surg Res. 2015; 101(1 Suppl): S139-47
- Pappas E., et al. Lessons learned from the last 20 years of ACL related in vivo biomechanics research of the knee. Knee Surg Sports Traumatol Athrosc. 2013; Apr, 21(4): 755-66
- AIS. Prescription of training load in relation to loading and unloading phases of training. 2015