Ankle and Foot Injuries in Gymnastics – A Complete Guide
Ankle and foot injuries are one of the most common problems gymnasts face. Depending on the study you read, up to 50% of all lower-body injuries in gymnastics occur at the ankle and foot. When you look at the sport, it makes sense. It is full of high impact forces, high repetitions, young athletes going through puberty, and has many cultural issues that might make it challenging to keep the ankle and foot joints healthy.
As a former collegiate gymnast, I’ve had my fair share of ankle injuries including 2 broken ankles, numerous strains/sprains, bone bruises, and microtears in my Achilles tendon. As a Sports Physical Therapist, Strength Coach, Gymnastics Coach, and researcher specializing in gymnastics, I’ve unfortunately worked with 1000s of gymnasts for foot and ankle injuries.
In an effort to help provide high-quality information to the gymnastics community, I wanted to create this “mega-blog” for people to use as a reference. I will provide all of my thoughts on common ankle and foot injuries and how to manage the stages of different injuries. I will also share how to safely progress back to gymnastics after an injury, and how to reduce the risk of ankle and foot injuries in our sport. I have spent hundreds of hours reviewing the literature on this topic in an effort to make this blog very high quality. So, throughout the blog I will provide links to the scientific literature, and a complete list of references below, for those who wish to really dive into the research.
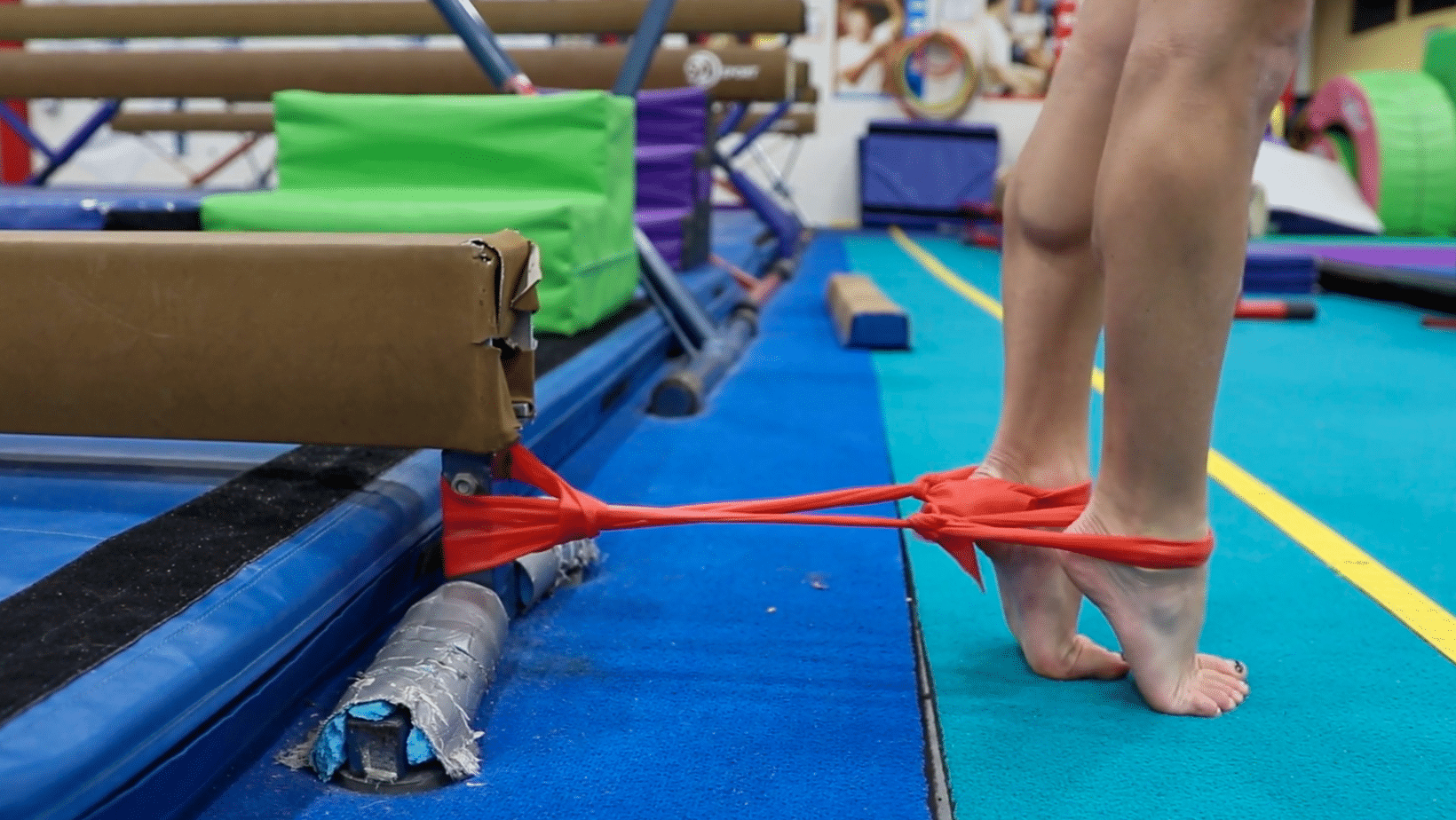
Table of Contents
In-Depth Courses for Gymnastics Coaches and Gymnastics Medical Providers
Before going down the rabbit hole, I know that many people want a “step by step” instruction guide for fixing gymnastics ankle injuries. If you are a gymnastics coach, we have 40+ of webinars, handouts, and discussion boards inside our online gymnastics education group The Hero Lab. We cover everything from flexibility, to strength, to culture, and more. For Gymnastics Medical Providers, we have an 8.5 hour PT/AT CEU approved course where I will teach you exactly how I treat gymnasts for hip, knee, and ankle injuries called Evidence-Based Evaluation and Treatment of Lower Extremity Injuries in Gymnasts. You can check them below out if that fits your fancy.


Also, if you prefer to listen to this in podcast form, or watch it in video form, you can check those out here!


How Common Are Ankle/Foot Injuries in Gymnastics?
To help wrap your head around just how common ankle or foot injuries are in gymnastics, it’s good to look at what is called epidemiology studies. These are studies that look at how often certain injuries occur in different groups of people. Here are some of the studies that are helpful to frame this conversation.
- 2019 Systematic Review by Thomas & Thomas of 12 studies, containing 843 gymnasts
- 51% of injuries occurred in the legs of gymnasts (hip, knee, ankle, foot).
- Ankle sprains were one of the most common injuries across all levels, ages, and disciplines.
- O’Kane 2011, 96 Club level gymnasts Level 4-10
- 19% of injuries were to the foot, 19.3% of injuries were to the ankle
- Westerman 2015, a 10-year study of 121 gymnasts in the NCAA
- 39% of injuries were to the foot and ankle
- Freshman had the highest rate of injuries
- Kerr 2015 in NCAA Gymnasts, 11 programs with 418 injuries over 5 years
- 50% of injuries were in the lower extremity
- The ankle/foot/Achilles was the most common injury location
- Floor was responsible for the most injuries, due to repeditive impact
- Most injuries required at least 3 weeks of missed practice or competition
- Paxinos 2019 of 156 elite gymnasts over 10 years
- 16.5 injuries were to the ankle, 16% of injuries were to the foot
- Kolt 1999 of 64 elite gymnasts over 18 months
- 31.2% of injuries were to the foot and ankle
- Salun et al 2015, 21 year study of 3681 injuries from elite/intermediate/novice level
- 17.6% of all injuries, totally 647 injuries
Why Are Ankle/Foot Injuries So Common in Gymnastics?
With stats like this, it’s a bit terrifying to see just how bad ankle and foot injuries are in gymnastics. Speaking from experience, I can tell you first hand these types of issues plague gymnasts for their entire career and beyond. Many gymnasts sadly just resort to using roll after roll of tape on their ankles or take massive amounts of Ibuprofen to help ‘just deal with’ stabbing ankle pains that occur on every landing.
I personally feel that this is not something we should just accept as part of gymnastics. Gymnastics is hard, and will certainly come with bumps/bruises like all sports. I’m not saying that it’s dangerous for kids to do gymnastics. There are hundreds of amazing coaches and gyms around the world that do an incredible job of developing athletes over their entire careers.
I’m simply saying we must have an honest, direct conversation about what the major contributing factors are for ankle and foot injuries in gymnastics. That allows us to make science-informed decisions about how we can make changes and reduce risk. Which is where we are heading next.
High Impact Landing Forces
Across the majority of the studies above, almost all of the foot and ankle injuries came from various forms of impact. In gymnastics, there are different forms of impact. One is the “technique” based impact that comes with tumbling, punching, or bounding. This involves a more stiff, rigid, body posture that allows the gymnast to utilize the equipment (springs in spring floor or board, balance beam, etc) to create bounce and perform skills.

The other type of impact comes from landing skills or dismounts. This should involve using a traditional squat-based movement to help absorb extremely high forces (more on that later). The forces of sprinting are also common in gymnastics, but these are not nearly as high as landings.
The forces of gymnastics tumbling and landings are massive, ranging from 15-18x bodyweight (more in this textbook here and here). In fact, the highest recorded forces that we know of were measured at the ankle joint during the take-off of a double back on floor and reached up to 23x bodyweight (more in this textbook here and here).
Keep in mind, this data mostly comes from controlled settings and definitely does not reflect all of the “real-life” situations of gymnasts landing short, more on one leg, or awkwardly. This is just a tough reality that we have to face in gymnastics, but if we face it head-on we can look at ways to help like strength and conditioning.
High Impact Repetitions
Along with high-impact forces, another reality of gymnastics is that it is HARD. By hard, I mean the skills themselves are extremely challenging to learn, master, and compete. Even the most basic skills take years to master. Due to how hard the skills are, it often takes thousands of repetitions to make progress. With the proper dosage, progression, and monitoring, these impact forces can be beneficial and help athletes adapt.
Unfortunately, for many in the sport, this type of approach might be lacking. As a result, they may end up taking thousands of high-impact repetitions per month without proper strength, skill technique, or recovery. This can create a situation where various tissues in the foot and ankle get overused and start to develop pain or injury. Or, it could create a situation where the athlete is exposed to really high impact forces before they are mentally or physically ready, creating an acute injury. With this in mind, we must look to education, the use of matting to buffer forces, and strength & conditioning to help combat risk.
Gymnasts Being Young & Pre Puberty
Harsh reality number 3 – the majority of athletes training in gymnastics are children. Despite ages trending upward for the world and Olympic teams, the vast majority of people competing in gymnastics are under the age of 16. They are young kids, who have yet to fully develop physically or mentally. This means, according to great research and textbooks, they are nowhere near their peak strength, power, or cardiovascular capacity. Not to mention, their growth plates are wide open and very vulnerable to injury. If gymnasts are not developed enough or lack the physical preparation to protect their ankle joints and open growth plates, injuries might stack up fast.

Gymnastics is a very unique sport where very young kids ages 8-12 are asked to perform very high force skills, in high amounts, and are training 20+ hours per week in some situations. In some areas of the sport, particularly those trying to get on the pre-elite/elite or NCAA track, it can create a situation where pre-pubertal athletes are training high force skills, in high repetition, well before their bodies are physically or mentally capable of handling it. This is where expert coaching, training plans, and pacing comes must be a priority.
Sport Culture – Early Specialization
One of the most important, yet most challenging factors to make changes in is gymnastics culture. The last five years have clearly shown us that there are many dark corners of a gymnastics training culture that exist in “old school”, archaic methods being used. There has been a massive amount of scientific data published around early specialization (here and here), year-round training (here and here), strength and conditioning (here and here), workloads (here and here), that have yet to make their way into mainstream gymnastics training.
Early specialization, when an athlete chooses to only participate in one sport, is one of the biggest concerns. It is common to hear gymnasts being told they will ‘miss their shot’ if they don’t only do gymnastics from a young age. While I do believe that gymnasts, particularly those with high-level goals, may need to specialize earlier than most sports, asking a 6 or 7-year-old to only train in gymnastics and not experience other sports is asking for disaster.
There is great evidence that this is concerning for increasing the risk of burnout, overuse injuries from repetitive movement patterns, and that it may negatively impact their overall athletic potential long term. The majority of the literature suggests that 14 or 15 years old is ideal for specialization. With that in mind, I think that may be unrealistic for many gymnasts, and that 10-11 might be a better target. But hearing about gymnasts specializing at 8 years old, as studies including one in the NCAA I was part of have suggested, is definitely concerning for all injuries but ankle/foot injuries in particular. This is something our sport desperately needs to talk about and change to protect young at risk gymnasts.
Sport Culture – Year-Round Training
Year-round training is another concerning cultural phenomenon that continues to persist in gymnastics. As with early specialization, there is an abundance of research across many sports (more here , here, and here) suggesting that athletes who train more than 9 months out of the year in a single sport are at elevated risk of injury and burnout. This has been well studied in baseball, which is a sport I’m fortunate my mentors Mike Reinold and Lenny Macrina were pioneers in alongside current studies like this.
I strongly feel that creating relative off-seasons, using periodization, and utilizing cross-training are crucial for reducing ankle injury risk and optimizing performance. The reality of our sport is that there has never been a time when gymnasts followed evidence-based guidelines around recovery, offseasons, and science-based work to rest ratios.
My hunch is that remodeling our year-to-year approach, shortening competitions seasons, and giving athletes a relative off-season after their hardest meet, would yield massive improvements in health and performance. I think the COVID pandemic is a further support piece of this, where many gymnasts said that after 2-3 months off, they felt the best they have ever felt mentally and physically. I don’t think it’s wise to give gymnasts extended periods of time fully off each year (3+ months for example). Hower, 4-6 calculated weeks would likely be incredible for athletes, coaches, and parents.
Lack of Science-Based Strength & Conditioning Methods
This is something that applies to all gymnastics injuries but in particular lower-body injuries of the knee and ankle. As mentioned, depending on the study up to 51% of injuries in gymnastics are in the lower body with very high proportions coming from the knee, ankle, and foot. There are two huge modifiable factors, strength & conditioning and teaching proper landing patterns, that are still not being utilized to their fullest potential in gymnastics.
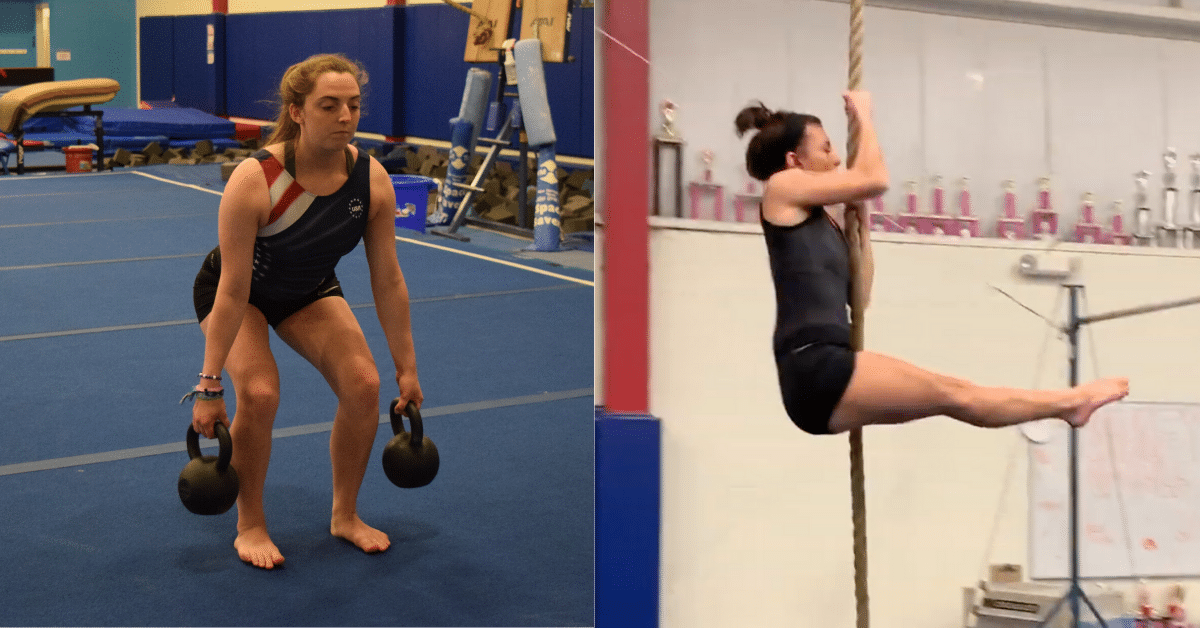
Based on great literature (more here, here, and here), it is clear that a properly done, properly coached, and properly progressed strength and conditioning program is beneficial for performance and reducing the risk of injuries. This includes a combination of both external weight lifting and bodyweight strength work. Taking this one layer further, a lower body strength program can be insanely beneficial in a jumping/impact-based sport like gymnastics.
Despite the abundance of evidence, there is still a huge percentage of gymnastics professionals who feel that gymnasts should not be lifting weights. They fear myths and misunderstandings about weight training, believing that it will make gymnasts “bulky”, less flexible, and cause injuries. However, a closer look at the literature show this to be largely false, given the program is properly implemented and coached with an aim of improving explosive power.
As a result of this cultural barrier, many gymnasts do not get the adequate leg strength and capacity needed to handle the high-impact forces. This is often where we get into trouble of both overuse and acute injuries to the foot, ankle, and knee. For more information about this topic check out this popular blog post I wrote in 2016.
Also, if you would like to read my “Ultimate Guide to Gymnastics Strength” – you can check it out here.
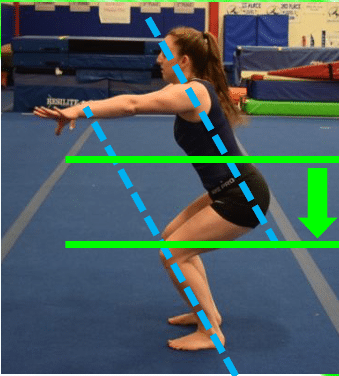
Improper Landing Techniques Still Taught & Used
Closely related to this is the ongoing cultural resistance to adopting science-based landing mechanics. It is unclear whether this comes from a lack of education, an ‘old school’ mindset, or a desire to mimic the esthetic type landing seen in ballet or dance. Howeer due to this, many people in gymnastics still teach use, and judge, based on a landing position that is not supported by science to ideally help dissipate high forces. Many gymnasts still land with their feet together, torso upright, hips tucked under, and in a ‘knee’ dominant patterns that may shift more stress onto the knee and ankle joints.

This is in contrast to the suggested landing pattern, supported by enormous amounts of data in the knee/ankle injury literature, of a squat based landing that has the feet hip-width apart, knees tracking in line with the hip and feet, and the allowance of squatting to parallel depth so various musculature can be recruited to buffer forces.
Until this becomes the gold standard for teaching gymnasts how to land in practice and competition, we may continue to see high lower-body injury rates. I recently gave big presentations to the coaches and judges in the NCAA about this topic that you can check out here.
Lack of Science-Based Workload/Wellness Monitoring Programs
Workload, athlete monitoring, and periodization are all areas of research that have become very popular in sports around the world. It is very common to hear about sports like soccer, basketball, and baseball utilizing specific workload tools to help plan and manage training volumes in athletes.
While there has been more conversation about workload management in gymnastics, the current approach still largely depends on a coach’s perception for decisions to be made. This was recently shown in Rhythmic Gymnastics but is likely the case in other domains such as artistic, trampoline & tumbling, and more.
If we hope to curb the amount of ankle/foot injuries in gymnastics, it is imperative that we look into better tools for external and internal workload tracking. Without knowing what the forces of different surfaces are on the foot/ankle, and how to keep a close eye on the training load gymnasts take, it’s like trying to fly a plane without any gauges or speedometers.
While this is evolving in gymnastics and is a field I’m actively doing research in (see below), the reality is we still have a long way to go.

Lack of Science-Based Flexibility Methods
While this isn’t as large of a factor in the ankle/foot compared to the hips or shoulders, it still is worth noting. There has been an abundance of new literature on the science of flexibility (more here and here), the most effective ways to improve flexibility, and what can be done to spare joints or ligaments while biasing changes in muscular tissues.
This matters in relation to calf flexibility, as well as lower-leg flexibility for proper landing patterns. To see positive progress, we must continue to adopt these new ideas and implement them in practice. If you are interested in my ‘complete guide’ to gymnastics flexibility, you can find that here.
Gymnastics Basics/Foundational Technique Sometimes Not A Focus
On the sport-specific side of things, it has to be mentioned that technology itself is a huge factor in injury risk for gymnastics. While there is not as much scientific evidence looking at different types of gymnastics skill techniques, it’s paramount the gymnasts are taught proper basics, foundational techniques, and progressions.

Without this, the forces of skills and the equipment can cause substantially more strain on the gymnast’s ankles, particularly in relation to tumbling, vaulting, and dismounts. This comes down to better coaching and education systems throughout the world, to share. the optimal technique and progressions to keep gymnasts as safe as possible.
Equipment Technology Progression
Lastly, there is no denying that the sport of gymnastics has become exponentially harder in the last 10 years as equipment technology progresses. The spring floor, the vaulting table, the trampoline beds, and other advancements have helped skyrocket the level of skills being performed. The double-edged sword here is that this also increases the average force the body takes.
While the landing surfaces and matting have also increased in their ability to protect athletes’ ankles and feet, the net increase in force is still substantially higher in today’s gymnastics environment. It also creates a small ‘ripple effect’ on the younger generations, where the nature of harder skills being performed means that more time, effort, and possibly starting to learn these skills at a younger age, also occurs. Coaches must be trained on how to use different equipment for proper progressions, and we also have to financially support gyms that need better equipment to keep athletes safe.
Basic Foot & Ankle Anatomy As It Relates to Injuries
I by no means am here to bore people with a dissertation in anatomy. But if we wish to make a change in the rates of ankle/foot injuries, we must first understand the anatomy that contributes to those injuries. This helps to understand the nature of common injuries and leads us down the road of helpful strategies to reduce risk.
If you want all the scientific textbooks and anatomy references to look up, check out this textbook, and research studies here here, and here.
Layer 1 – Bones
The main ankle joint is made up of three bones joining together. The ends of the lower leg bones make up the top of the ankle joint. The tibia sits on the inside and the fibula on the outside. These two bones sit side by side, connected by connective tissue, and their ends form a downward facing “C” shape.
Below this is the talus bone, which makes up the bottom of the ankle joint. The shape of the surface of the talus is rounded so that it articulates well with the downward “C” created by the tibia and the fibula. This joint, called the talocrural joint, is what allows the toes up and toes down motion of the ankle. It also takes a massive amount of the impact forces during running, landing, and skill work in gymnastics. The majority of the forces go through the tibia, and into the talus.
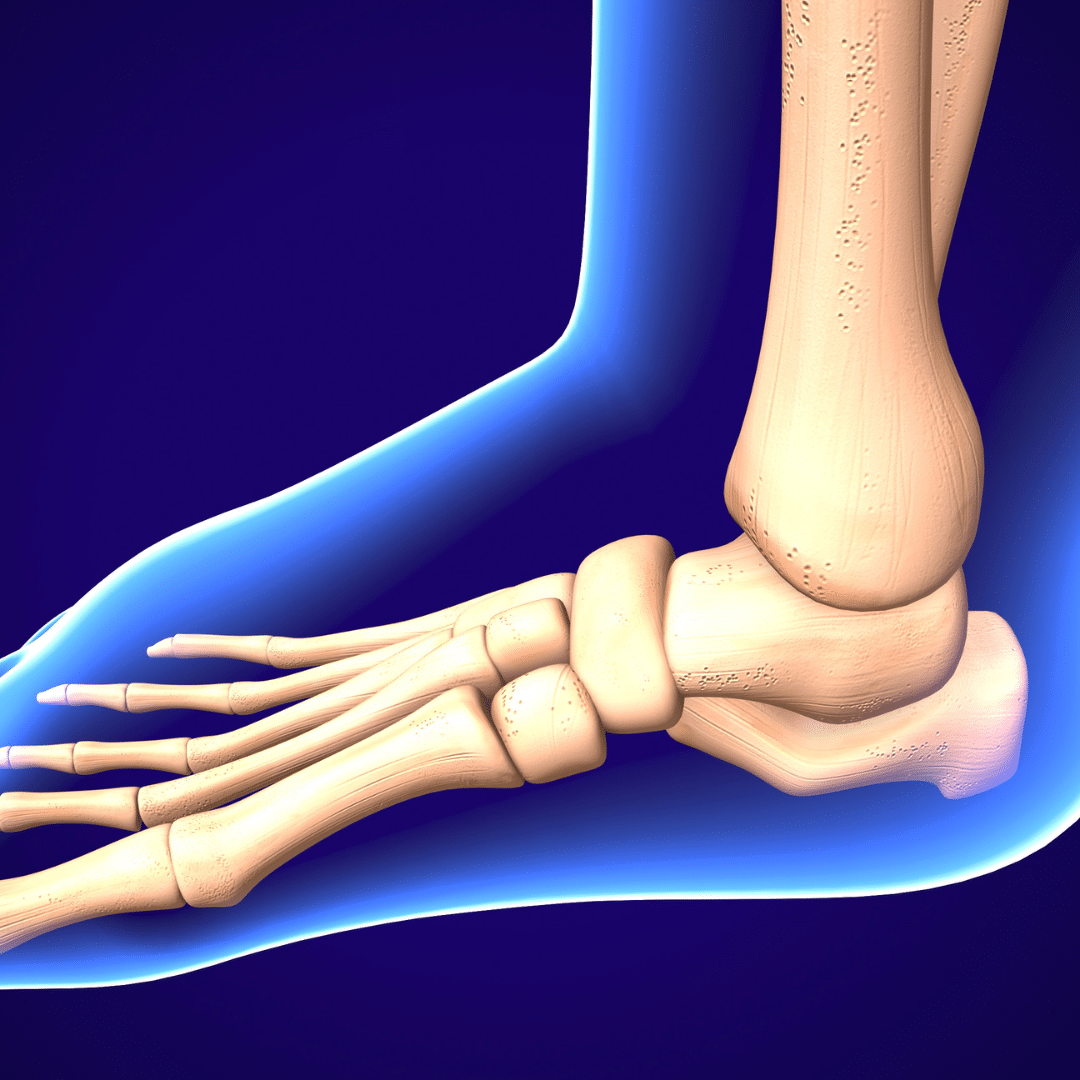
Below the talus bone is a third bone, the calcaneus. It also takes impact forces transmitted down from the bones above, but also helps provide side-to-side motion of the ankle. The connection of the talus to the calcaneus, called the subtalar joint, is what mainly allows the foot to roll in and out. When combined with bones in the foot, these joints allow for a more flat foot position (sometimes called”flat feet”) and a more curved foot position (sometimes called “high arches”).
Contrary to popular belief, it’s actually a good thing that the arches of the feet can flatten and rise. It allows athletes to produce and absorb forces that allow them to walk, run, jump, and land. Problems come up when someone gets ‘stuck’ into one of these positions, or lacks the strength or capacity to handle the forces.
Moving from the ankle bones are the foot bones. The foot is made up of many smaller bones connecting together. This allows the foot to be semiflexible, and move fluidly in and out of the arch positions mentioned above. It also provides many anchor points for various muscles that create lots of movement and force production. The first bone extending into the foo is the navicular, followed by the 3 cuneiforms and the cuboid. Then past this are the 5 main foot bones, the metatarsals, and finally the bones that make up the toes, the phalanges.
Layer 2 – Ligaments/Joint Capsule
To support the many different bones and joints, ligaments and joint capsules are necessary.
The main joint capsule of the ankle surrounds the joint made by the lower shin bones and the top of the talus. Think of this joint capsule as a thicker “saran wrap” around the entire joint, and filled with fluid. This fluid is called synovial fluid and serves to both provide nutrition and also help lubricate joint surfaces so that smooth gliding can occur during movements. There are also many smaller joint capsules surrounding the joints of the toes and other joints.

Ligaments are very important to help prevent excessive motion between bones and joints. We have larger, more notable ligaments and some that are a bit smaller between tiny joints. One of the main ligaments involved in ankle sprains is the one that connects the outer shin bone to the talus, the ATFL (anterior talofibular ligament). On the inside is a much larger, more thick ligament called the deltoid ligament.
There are many, many small ligaments connecting the various bones of the ankle and foot beyond just these. Rather than bore people going through them, I will discuss them as they come up to common injuries in the next sections.
It is also worth mentioning that there is a very dense band of connective tissue that travels on the bottom of the foot from the heel up to the front of the foot. It is called the plantar fascia and serves as a very supportive shock absorber and structure to transfer force during walking/running.
Layer 3 – Muscles / Tendons
Of more importance is knowing about some of the main muscles that support the ankle/foot, and help produce or absorb force. These are not only commonly involved in injuries, but also serve as a really great way for us to try and reduce the risk of overuse injuries by building strength.

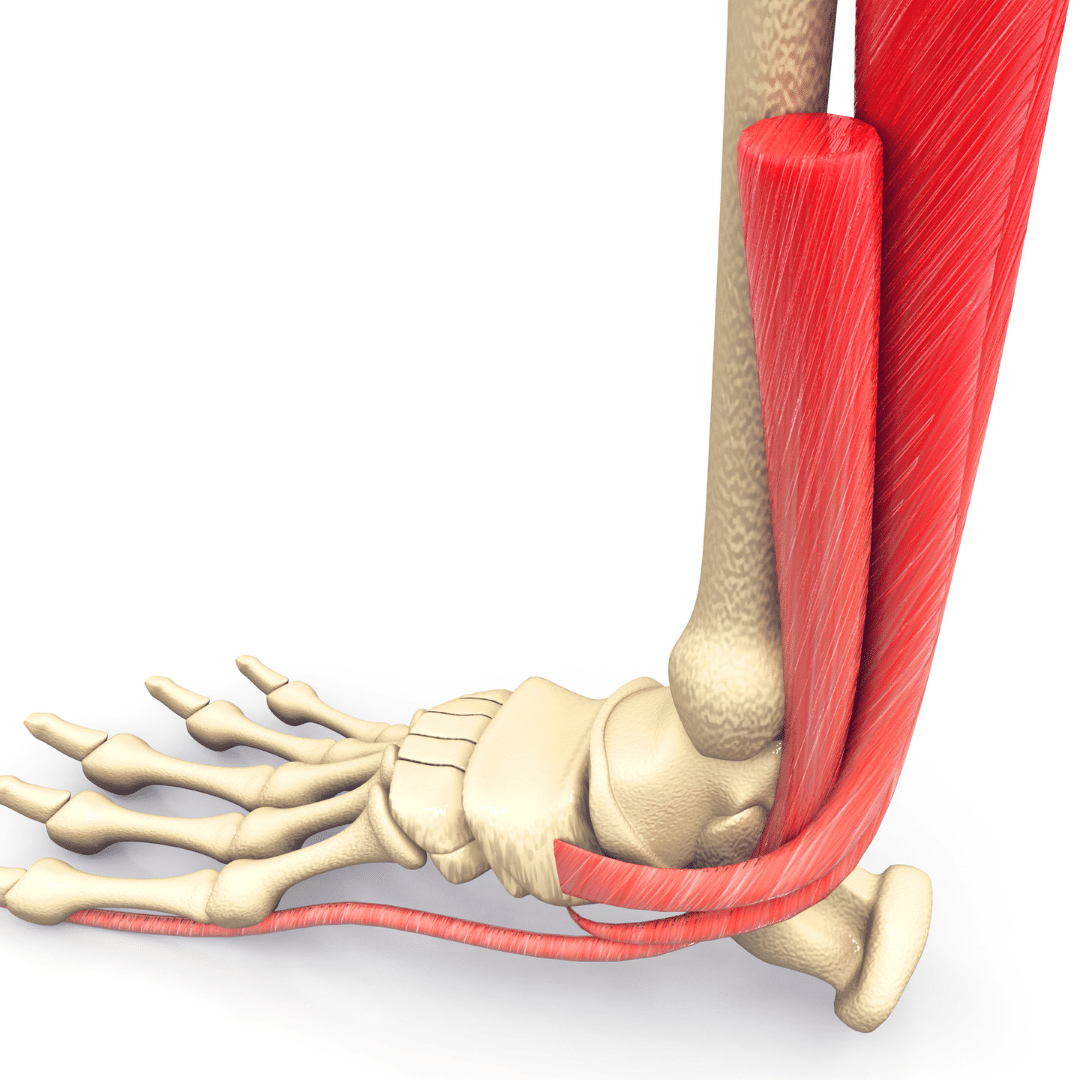
On the back of the lower leg are the calf muscles, which are very important in gymnastics. To muscles, the gastrocnemius and the soleus, combine together to form the large, thick Achilles tendon that inserts on the heel. It provides a massive amount of strength for push-off power in waking, running, and jumping. It also serves a huge role in absorbing tumbling and landing forces.
Moving more toward the inside of the lower leg is the posterior tibials muscle. It does sit somewhat in the back as well as the inside, but it runs down behind the large boney bump on the inside of the leg, the medial malleolus. This muscle is helpful for assisting the calf muscles above, but its more important role is to support the arch of the foot. It can also pull the entire foot down and inward. The tendon of this muscle wraps around the boney bump and travels under the foot through the arch. This allows it to not only help create the arch but also absorb forces during impact. There are also smaller muscles that travel from the back of this lower leg bone and attach to individual toes, allowing for curling and further arch support.
On the front part of the leg is the muscle that works in opposition to the posterior tibialis, the tibialis anterior. This muscle sits on the front and outside part of the shin, travels down across the front of the ankle joint, and attaches to the top of the foot. It pulls the foot up into a ‘toes up’ motion and also helps stabilize the foot during loading. There are also smaller muscles that travel from the front of the shin and attach to individual toes to help pull them up.
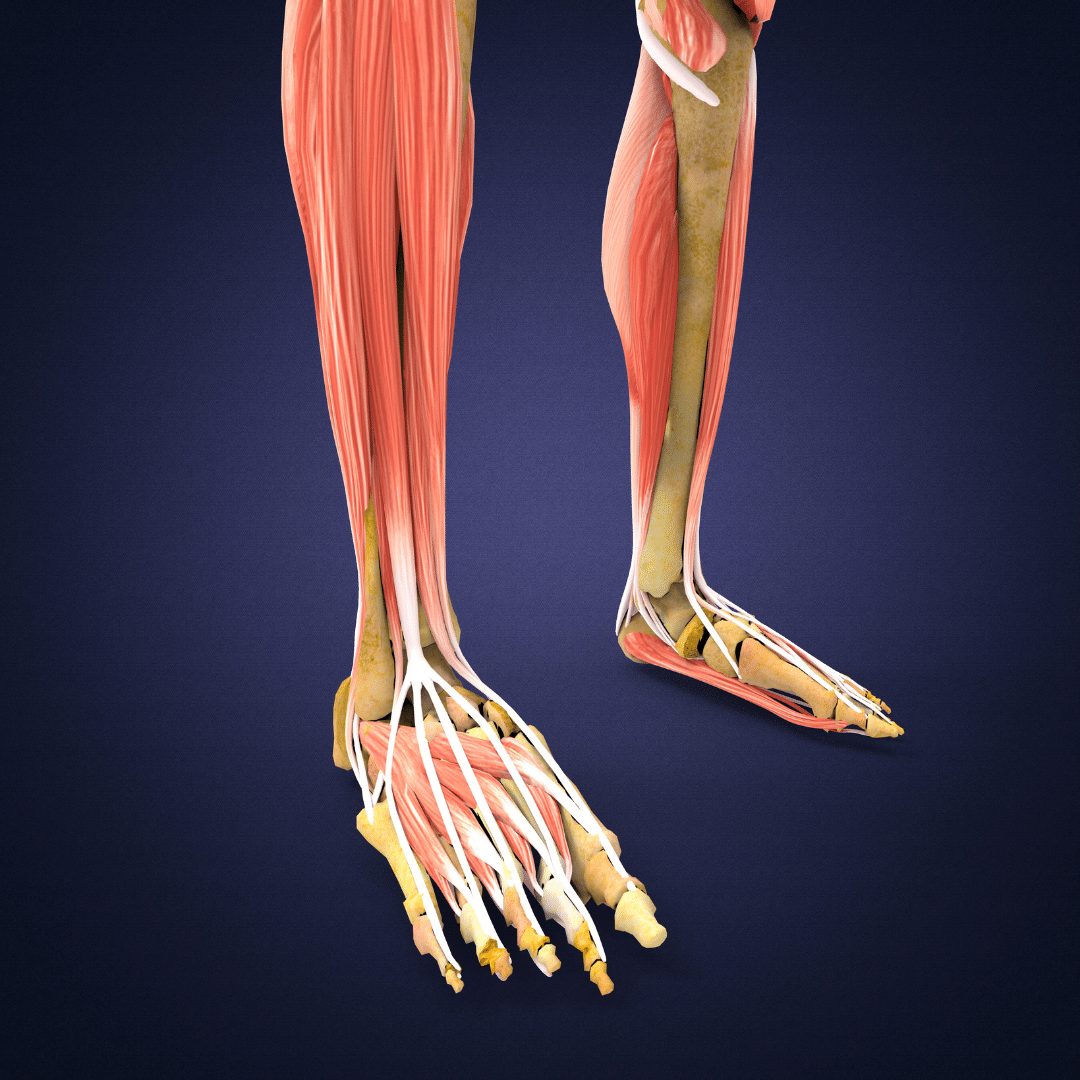
On the outside of the lower leg are the muscles that pulls the leg upward and out, the peronneals. There are two muscles working together that wrap around the boney bump on the lower leg, the lateral malleolus, and attach to outside foot bones. Along with moving the foot, these muscles are very important in helping to stabilize the foot and provide overall balance alongside the other ankle muscles and knee/hip muscles.
Lastly, there are a large variety of smaller muscles within the foot that provide to help move the toes, support the arch, and transfer force around. Some of the more notable ones are the lumbricles, the interossei, and flexor/extensor digitorum muscles. Similar to the ligament section, it’s beyond the scope of this blog to go into every single muscle as there are entire university courses on this. It would also be incredibly dry and boring for readers. I will bring up certain muscles of importance as they relate to injuries below.
Layer 4 – Nerves & Blood Vessels
Although we won’t be diving in too deep here, it is important to mention that there are large amounts of nerves and blood vessels that travel throughout the ankle and foot. Nerves help send/receive signals from the ankle structures. They also provide signals for muscle activity. Blood vessels are the main source of providing nutrients to the different areas in the foot and ankle. They also help transport waste products out of healing tissue along with the lymphatic system. Again, I will bring up specific nerves of blood vessels as they relate to injuries to not make things too complex.
Layer 5 – Kinetic Chain
While not a true ‘layer’, it’s crucial to understand that the joints above the foot and ankle play a huge role. Not only do they influence the movement of the foot and ankle, they also work in tandem with these other joints for gymnastics. As an example, the hip joint can drive motion at the knee, which may then change the types of forces put into the ankle. Say for example if a gymnast struggles with an overextended lower back position from stiffness in their hips, it may put more force on their ankle joints during landing.
What Are The Most Common Ankle and Foot Injuries in Gymnastics?
Now that we have a good background in the ankle and foot, let’s dive into the most common injuries in gymnastics and what causes them. It’s important to understand that generally, there are two different broad categories of injuries – acute and overuse. Acute injuries are when one incident causes the injury, and tend to be a bit more severe. These can include things like ankle sprains or falls that cause bone fractures.
Overuse injuries are when multiple incidents slowly cause an injury to accumulate over time. These can be things like growth plate irritations, tendonitis issues, and stress fractures. Looking at the research in a big picture, overuse injuries account for about 70% of all injuries in gymnastics where 30% tend to be more acute. That is a bit concerning, as that means there is a ton that we could possibly be doing to reduce these rates.
As we move through these injuries, I will follow the same “layered” approach to the anatomy above to help people better understand what is going on.
Ankle Sprains
When you look at the research, ankle sprains are by far and away the most common injury that gymnasts face. This is true across different disciplines, genders, ages, and levels. And putting together the pieces above, this does make sense. Given that gymnastics is a complex jumping and landing sport, athletes are exposed to thousands of impacts per month. The skills are difficult, the equipment is challenging to work with, and it comes with the nature of the sport.
Generally, sprains follow 3 categories of increasing severy. Grade I sprains are relatively benign, and just involve stretching of the ligament. There may only be mild swelling, bruising and discomfort with walking. Grade II’s are a bit more severe, and what people more commonly seek help for, as they involve micro-tearing of the ligament and joint capsule. These typically have much more swelling, bruising, and it’s painful to walk as putting weight on the ankle compresses the sensitive tissue. Grade III sprains are the worst scenario, as the ligament is truly torn and there likely is another tissue damage around the area. These typically are evaluated with an MRI, and possible surgery, to restore the ligament back. For more in-depth research information, check out this article.
Inversion Ankle Sprains or “Rolling In”

The main mechanism for inversion sprains is a ‘rolled ankle’ which usually refers to the ankle rolling downard and inwards. This usually occurs accidentally when athletes are running, landing skills, and doing punching or connection tumbling. When this happens, a few things occur which make ankle sprains challenging to get over quickly. From a boney point of view, when this rolling occurs there is often a forceful motion occurring at the ankle joint. On the outside of the ankle, the outer fibular bone may hit the surface very fast causing a bone bruise. On the inside of the ankle joint, the inner ankle bones may also compress and hit each other also causing bone bruising.
When these bones move rapidly beyond what they are comfortable with, it causes a lot of strain on the structures on the outside of the ankle joint. The ATFL (anterior talofibular ligament) is typically the most commonly injured ligament. The joint capsule around the ankle joint also is commonly overstretched. This, combined with excessive fluid build-up in the area, is often what creates the dull, diffuse achiness or soreness people feel long after the actual incident. It also may be why people struggle to get back impact if the proper healing timelines and rehab exercise progressions are not used.
With increasing severities of inversion sprains, progressively more tissue damage may occur, and thus a long recovery may be needed. With the increasing severity of sprains, more ligaments around the ankle might also be involved which extends the timeline for recovery (the CFL/calcaneal fibular ligament and PTFL / posterior talofibular ligament). These ligaments wrap around the back of the ankle, and if damaged will have lots of tenderness and lost ankle motion.
Eversion Ankle Sprains or “Rolling Out”

The opposite of this can also occur, when the ankle rolls outwards, leading to an eversion ankle sprain. While these are less common, then tend to be more severe and require more rehabilitation time. This is because the inside ankle ligament complex, the deltoid ligament, is much more dense and firm. This means while it takes more force to cause injury, it also is more challenging to heal. The same situation can also occur where a bone bruise occurs on the opposite outside part of the foot as those bones forcefully hit together. The same concepts apply above, with increasing swelling, bruising, or inability to walk/move being more serious.
High Ankle Sprains
Another more nuanced type of ankle sprain that occurs less commonly, is a high ankle sprain. This typically happens with extreme toes up or “crunched” ankle positions happen rapidly. I’ve seen this happen often when a gymnast miscalculates their tumbling distance going into the put, and half their foot lands off the edge of the tumbling surface when they try to take off. I’ve also seen it happen with awkward or under rotations in landings, causing the foot crunch into an up and out position.
Unfortunately, they are more severe and this is where most people come up with the idea that sometimes a broken bone might be easier to deal with as it heals faster. Sometimes bad high ankle sprains can take up to 3+ months to heal because the ligaments and tissue that holds the lower leg bones together are slow to heal. A rule of thumb used is that for every 1″ above the ankle joint these injuries occur, it’s an additional 1-2 weeks of healing that might be needed. The tissue holding the lower leg bones together, the syndesmosis, can become extremely irritated and have a tough time tolerating impact. Also, the bones themselves often get quite a bit of bruising, as well as the ankle joint capsule. Although rare, these can be really frustrating for athletes.
“Crunched” Ankles (Talocrural Impingement)
I’ll be honest here in saying that while ankle sprains are reported as the most common injury in research, I actually think that this is the biggest problem all gymnasts deal with. While we can have ankle sprains from this crunched position as mentioned above, I think the bones themselves take way more of a beating over time. I think that ankle sprains, like many other areas of the body, are the most reported because they are challenging to not speak up about. When someone sprains their ankle, it’s pretty obvious and there are clear issues that result (limping, swelling, bruising, etc).
Crunching your ankles on the other hand, tends to be something that gymnasts wrongly try to shake off or simply plaster ankle tape around to make it go away. Also, unfortunately, this is a cultural problem with it just being ‘part of the sport’ similar to back pain. I disagree that this is something to just casually work through. Accidents happen, but if someone consistently keeps jamming their ankles we need to take a big step back and revisit basics, technique, strength, fatigue management, or goals to solve the root cause.
That said, lets’ break this injury down. What is actually happening during this injury is that the bones that make up the ankle joint, mainly the tibia and the talus, are forcefully smashing against each other during short or not ideal landing situations. This is why it’s called talocrural impingent, as these two bones rapidly crash into each other impinging soft tissue structure and creating injury.

In minor situations, the bones hitting against each other cause bruising and boney inflammation. Also, the ligaments and joint capsules that are caught in between this forceful compression become damaged and inflamed. This is what creates the ‘pinch’ sensation during the landing that hurts so bad, and why it’s painful to walk, run, jump, or land after. Generally, if this happens by accident and you respect it, it can resolve in a week.
In more severe situations, or when repeated ‘crunching’ events happen over and over, things can get much worse. For one, the bones repeatedly compressing the ligaments, joint capsules, and tendons in the front of the ankle progressively damage them more. This can lead to chronically painful ankle joints, losses in the ability to use the muscles, or lots of swelling within the ankle joint. Along with this, with repeated impacts, the joint surfaces themselves may start to develop boney overgrowth, as the body responds to the high force by laying down more bone tissue to handle the forces. This is called “wolf’s law” and is commonly seen in the knee with Osgood Schlatters. While it’s good in theory, in the long run, it can create more problems with mobility or irritation.
Also, remember that the top of the talus bone has cartilage on it (the talar dome) that when repeatedly hit in the same spot can get very damaged. This can cause one localized area to get inflamed, not heal, and for the cartilage or bone to actually start to decay. This is called osteochondritis dessicans (OCD) and is a much more serious condition, as you can not replace the cartilage you are born with. Along with damaging the cartilage and causing pain or lost function, small fragments of the cartilage or bone can also break off, and become loose bodies inside the ankle joint. This is problematic because it causes pain, but also because it can cause more damage during weight-bearing and significantly limit ankle mobility.
This situation almost always lends itself to a huge restriction in training ability. Over time, many older gymnasts may be forced to stop doing harder floor/vault skills, dismounts, or stop training floor/vault together. Not to mention, as things progress and get worse, many athletes require surgery to remove loose bodies, try to promote healing in the cartilage (microfracture), or actually replace the missing cartilage with a bone plug graft from another area in the body (mosaicplasty or OATS procedure). These surgeries are very challenging to go through and recover from, often requiring 6-9+ months to come back from.
To help out with this pain, gymnasts must work on technique or revisit basics to stop landing short. They must have proper skill progressions, and also mental confidence to get skills around fully and use a proper landing pattern. Along with this, gymnasts must have the proper ankle flexibility and lower leg strength/power. This allows them to not only complete skills fully, but also have the capacity to handle impact forces. Should an accident occur that causes this, typically 2-4 weeks of rest followed by regaining mobility, then regaining ankle strength (more below), and returning to softer surfaces is needed.
Growth Plate Inflammation
Sever’s Disease (Calcaneal Apophysitis)

While there are many growth plates within the foot and ankle that can become painful in gymnasts, by far the most common that people struggle with is the growth plate in the heel. This growth plate located on the back/bottom side of the heel is where the large Achilles tendon inserts to. In most children, this growth plate does not fully close and becomes firm/hard bone capable of handling these high forces until 13-15 years old. This means it is very vulnerable to become inflamed and irritated if overused and lacking strength and flexibility occurs.
Remember that the gastrocnemius and the soleus are two very large, powerful muscles that come together to form the Achilles tendon inserted onto the heel’s growth plate. It takes a massive amount of force and also is used 1000s of times per month in gymnastics with running, jumping, landing, tumbling, vaulting, and dismounts. So with less severe irritations, the growth plate can become inflamed causing lots of pain, limping, and swelling.
Bone pain is one of the most painful things for a child to experience, so it’s extremely uncomfortable. If problems are not addressed right away, or gymnasts ‘push through’ without speaking up, things can progress to be even worse causing a stress fracture of the heel. This requires much more time to heal and time away from gymnastics, so it is imperative issues are caught early and dealt with head-on.
As mentioned in the introduction section, it is common in gymnastics culture for gymnasts aged 8-12 to specialize in gymnastics, train year-round, and start training very high-level skills requiring lots of repetitions. If we do not respect natural growth and maturity, properly pace young gymnastics in their pre-pubertal years, use softer impact surfaces, and delay the competing of very high force skills, it is easy for Sever’s disease to plague gymnasts for many years. Thankfully, with great coaching techniques and lots of focus on strength, great technique, and proper progression, the risk of long-term problems can be reduced.
For those trying. to get rapid pain relief from Severs, I do find that a combination of compression wraps, light soft tissue work to the calves, and cold water soaks are helpful. If someone is in significant pain, a heel wedge to take pressure off the bone for a few days may help. While light stretching does help, we have to be careful not to over-stretch and pull more on the bone. Also, time away from impact and a slow 2-4 week return to impact is crucial. For more information, check out. this popular YouTube video I made on Severs.
Iselin’s Disease (5th Metatarsal Apophysitis)
Another growth plate injury of the foot, albeit less common, is Iselin’s disease. This is a similar phenomenon to Sever’s disease in the heel, but occurs at the base of the 5th metatarsal located on the outside of the middle foot area. One of the peroneal muscles that wrap around the back of the ankle bone attaches to this growth plate. With repetitive use of the ankle muscles jumping, running, landing, and balancing, it is common for inflammation of the bone to occur.
Similar to Sever’s disease, it’s crucial that injuries to this area are communicated and dealt with right away. This growth plate can quickly become damaged to the point of a stress fracture, and serious issues can occur if the fracture gets so far gone that it is unable to heal (called a malunion). It is also possible that with persistent irritation, it may become more susceptible to traumatic fractures during landings or impacts. Similar principles to the heel occur, where time away from impact, full healing, and a progressive strengthening/gradual return to impact program are necessary.
Tendonitis/Tendinopathies
In the bigger picture, it’s helpful to follow Jill Cook’s work here and view tendon issues as existing on a continuum. This paper, this paper, and this paper are great to read and are what the following sections are based on.
Tendonitis
On the left side of the continuum, you have the very acute and ‘hot’ tendon injuries, often called tendonitis. This typically occurs in a single incident or tipping point of pain, bringing on sudden very intense bouts of pain. In most cases, this typically has a true inflammatory component as the tissue is suddently overloaded with a high force movement or some sort of sudden load spike.
Tendonopathy
In the middle of the continuum are tendinopathies. The role of true inflammation has been combatted in the current research, and it is mainly thought not that an imbalance of workload placed on the tendon, and the tendons lacking the capacity to handle it, create a progressive degenerative process within it. This could be due to the excessive workload being placed on it without enough recovery between loading bout (lots of sudden impacts in a few weeks/ months time). It could also be related to a lack of strength, making the tendon less able to tolerate high forces.
There also may be other factors like nutrition status, technique, genetics, unique anatomy, and more. Given all this, what is typically happening here is that the tendon itself starts to change, and the tissue that makes up the tendon (collagen) starts to become not the healthiest type that is able to handle the load. This could create a situation where the nerve ends start to grow in the tendon creating pain, or that due to its lowered capacity to handle the load, high force impacts or over-stretching of the tendon can cause microdamage and irritation. To help address this, typically a reduction in tendon stress is needed for a short period of time while exercises and strength drills can be used to increase the tendon’s capacity and possibly promote healthier collagen tissue to remodel.
Tendon Rupture
At the far right side of the continuum would be tendon failure, also referred to as tendon ‘ruptures’ or ‘tears’. This is a very devastating situation, where the tendon has gone through so many cycles of microtrauma or degeneration, that in one moment of tissue overload the tendon reaches its failure point. As I will discuss below, this, unfortunately, is seen in the Achilles tendon for many high school, NCAA, and elite gymnasts. While many people say these happen ‘out of the blue’, the reality is that this situation has likely slowly developed over years and years of loading. While we don’t know the exact risk factors leading to tendon failures, there is some growing literature to brainstorm what might be going on.
These injuries are much more devastating, requiring surgery to repair the tissue, extended time away from gymnastics to rehab, and a gradual return to sport progression being used. Not to mention, it dramatically impacts the athlete’s mental health and performance for the rest of their career. Knowing these issues exist, it’s crucial for people in gymnastics to look at the entire spectrum of tendon issues from the younger ages all the way to the later ages, and consider what can be done to mitigate excessive damage from occurring.
Achilles Tendonitis/Tendinopathy

The most common issue gymnasts face related to this is within the Achilles tendon, located on the back of the calf and insert onto the heel bone. As mentioned, when gymnasts are younger and have open growth plates the bones of their heel are not quite fully formed. This makes it the most vulnerable point, and typically what is the limiting factor for loading. It’s not to say that the Achilles tendons of young gymnasts may not be getting injured, it’s just that the bone typically is what becomes painful first.
However, as athletes mature and their growth plates close, the force overload may then change and start to switch to the Achilles tendon. Remember that the highest recorded forces in gymnastics occur at the ankle joint, measuring 23x bodyweight. The calf muscles, and as a result the Achilles tendon, are some of the main muscles that work like crazy to help handle those forces. This can produce cycles of pain, irritation, and lost strength which must be treated with workload modification and strength progressions to rebuild the tendon’s capacity.
During tumbling on the spring floor, impacts on vaulting boards, jumping, sprinting, and dismounts, the Achilles tendon takes an insane amount of force. If proper workloads, practice planning, strength programs, technique/progressions, and rotation of soft to hard surfaces are not used, it is very easy for the Achilles tendon to get irritated creating tendonitis or overtime, tendinopathy.
Personally, I find that these injuries tend to need 2-4 weeks of relative rest away from impact, followed by 2-4 weeks of progressive strength room. I find that seated calf raises, standing calf raises, and bent / straight knee tiptoe walks are my go-to’s for early loading. A special emphasis on eccentric loading can be useful. Following that, a slow return to impact using pogo hops, scissor hops, in and out hops, hurdle hops, and sprint work can be done.
Posterior Tibials Tendonitis/Tendinopathy
On the inside of the ankle, the posterior tibialis muscle starts on the lower leg bone and wraps down behind the ‘bump/ of the ankle, the medial malleolus. This tendon then goes down the foot and underneath across the arch. Remember that along with helping point the foot, this muscle has a huge role in controlling and supporting the arch of the foot. So during walking, landing, and impact, it works very hard to prevent the arch from collapsing and the foot flattening out too much.
Due to its huge role in buffering impact forces and helping to produce jumping/running power, it can frequently become irritated. This is particularly true under conditions of rapid stretching and contraction (called eccentric contractions) that occur in tumbling or dismounts. The tendon wrapping behind the bump of the inner ankle bone and going under the foot allows it to do a great job supporting the arch, but also subjects it to very high forces repetitively. Furthermore, right next door to this tendon is the posterior tibialis nerve, which can become irritated under these high-impact situations and contribute to pain.
If someone has very stiff ankle joints or limited ‘toes up’ ankle flexibility, it can sometimes contribute to the foot flattening out and causing more pressure on this tendon. Due to this, along with reducing impact load, strengthening this area directly, teaching proper technique, and modifying hard surfaces, we want to make sure we improve ankle mobility to take some stress of this area. Along with the exercises above in the Achilles section, I find both slant board arch drops and heel raises with a lacrosse ball squeezed between the heels are useful.
Peroneal Tendonitis/Tendinopathy
On the opposite side of the foot is the peroneal muscles and tendons on the outside. Again, these muscles work to pull the foot outwards, but they also are extremely important to help with stabilizing the ankle during landings, particularly those on one leg. They also work with the other foot muscles to produce for needed for running and jumping.
As athletes grow older, the growth plate in the outside of the foot that one of these tendons insert into closes, again shifting the stress more on the tendon-like with the Achilles. Due to this, similar issues can come up where this tendon starts to become irritated, or possibly break down in its ability to handle the highest forces (more research here and here). As we will discuss below, dealing with these issues is similar to other tendon issues. Workloads must be modified, we must strengthen the area, and find ways to change the surface as we slowly rebuild impact volume.
Plantar Fasciitis
Although not truly a ‘tendon’ issue, I felt it was important to mention plantar fasciitis around this section. The plantar fascia is a super dense collection of connective tissue that is under the foot, starting from the base of the heel and attaching to near the toes. It serves to help support the bones and arch of the foot, while absorbing and help transfer force during motion. The main factors that contribute to plantar fasciitis are sudden spikes in impact workload from hard surfaces, strength issues of the inner foot and leg muscles, and possible mobility issues within the ankle or first toe.
If this occurs slowly over time through multiple bouts of irritation, micro-irritation may occur within the connective tissue leading to pain and an inability to handle force. Dealing with these requires correcting the issues of high impact workload while loading the area through various calf or single-leg exercises. Specific mobility drills for the ankle and big toe can also be helpful during the rehab process.
If this occurs in one sudden rapid instance, say if a gymnast lands with the heel off the edge of a pit while tumbling, a torn plantar fascia can occur. This typically is much more severe, creating swelling, bruising, and the need to offload the foot with a boot or crutches for a period of time.
Many of the same exercises that are used to load the Achilles tendon can also be really useful to rebuild plantar fascia capacity. I also find that single leg exercises, such as step ups and RDLs, can be useful here. Of particular importance is the slow return to impact through low medium, and finally high impact. I tend to find hurdle hops, box jumps, and sprinting progressions are useful here.
Achilles Tears
I wanted to make sure I included a specific section on Achilles ruptures, as it continues to be a massive problem in gymnastics. It is typically seen in late high school, NCAA, or elite gymnasts as mentioned. As a study I was a part of suggested, the majority of ruptures occur on floor during backward tumbling skill take off. There are also some injuries that occur on vaulting, mainly in Yurchenko style vaulting.
There are many possible factors that can contribute to Achilles ruptures including technology progressions, training all around or elite levels, competing high-level skills when young, nutritional influences, skill technique, unique anatomy, and more. We are at the beginning of exploring the issues that may contribute to Achilles rupture.
That said, due to how devastating these injuries can be, we must try to do our best to reduce the risk of injury. Some of the main mechanisms for this are through careful impact planning and workloads, looking at how different sprint floors may contribute to injury risk, using very robust strength programs, communicating openly about the start of tendon pain or soreness, changing the culture to not push young gymnasts too fast too soon, science-based nutrition education, and focusing on excellent foundational techniques for basics. As more time passes, I hope we can learn more about specific strategies to offer ways to reduce risk.
For a very deep dive into this topic, check out these two large articles I wrote on Achilles Tears in NCAA Gymnastics (Part 1 here and Part 2 with Jill Cook here)
Shin Splints

Another very common, and often limiting, injury that young gymnasts struggle with is shin splints. This occurs when the muscles that attach to the shin bones get used repetitively, leading to inflammation of the point they insert called the periosteum. The repetitive impact, combined with the repetitive jumping/landing/running causes the bone itself to get irritated. This most commonly occurs when there is a sudden spike in impact or running workload, (lots of new plyo conditioning, lots or hard surfaces or routines in a few weeks). This situation causes not only a rapid increase in impact but also a rapid increase in the number of contractions the muscles around the lower leg take.
These typically can be broken up into two main versions, one in the front of the leg (anterior shin splints) and one in the back of the leg (posterior shin splints). They are collectively sometimes referred to formally as Medial Tibial Stress Syndrome. The front of the leg version most often involves the tibialis anterior, and the extensor muscles whereas the back of the leg version most often involve the soleus, posterior tibialis, and flexor muscles.
In less severe forms, the muscle itself and mild irritation of the bone from microfractures create pain. As things progress, the microfractures become larger stress fractures and can possibly lead to true tibia fractures that are clearly more serious.
Stress Fractures and Various Bone Fractures
Navicular, Jones, and Metatarsal Fractures
Progressing normally from microfractures/stress fractures of the shin, are various other types of stress or acute fractures throughout the foot and ankle. There are many different variations that occur causing issues. Most obvious are accidental fractures that are challenging to avoid. This can happen when awkward landings occur, or the pure accidental nature of gymnastics causes sudden contact with the equipment.
The sudden impact can cause the long bones of the feet, the metatarsals, to suddenly fracture. This can happen to any of the long bones, but the most known one occurs in the outer 5th metatarsal, called a Jones fracture. This also sometimes occurs on the inside of the foot, in the navicular bone. It’s of particular importance that the navicular fractures are allowed to heal fully, as returning too early can create much bigger problems that sometimes require surgery with pins to correct.
In reality, any of these bones can suddenty fracture, or accumulate stress fractures, if the right conditions occur. While they have different nuances to the types of braces, boots, or specific treatments that are used to immobilize them, they all mostly follow similar guidelines of allowing a few months to heal and then regaining mobility, strength, and capacity around the area.
Lisfranc Fractures
One particular injury worth mentioning is a Lisfranc fracture. This is an injury to the first toe that occurs when forceful axial loading occurs to the toe in an extended position. While it does involve a fracture or dislocation of the 1st foot bone, it also often involves a sprain or tear of the ligament that connects the 1st and 2nd-foot bones together. This is what makes this injury much more severe, often requiring surgery to reduce the bone, stabilize the fracture, and reconstruct the ligament. If a gymnast is to land forcefully in a high toe position and has swelling, bruising, and pain, it’s important to get an x-ray to rule out this fracture.
How Long Do Ankle and Foot Injuries Take To Heal?
Respecting The Body’s Healing Process
The question that I get from gymnasts most when treating them for ankle or foot injuries is – “when can I go back to gymnastics?” I completely understand athletes wanting to get back to training as fast as possible. It was the same for me as an athlete, and the coaching side of me certainly knows the challenge of having an athlete at practice hung up by these injuries yet wanting to make progress.
That said, we can not magically speed up basic human biology. There are certain things we can do to accelerate, assist, and enhance the natural healing process. But at the end of the day, we have to understand and respect the body’s healing timelines. There is a base timeline for various tissues of the body, and when looking at the literature a realistic timeline for various degrees of injuries. Unfortunately, these don’t change even if we are in the middle of competition season or ahead of a very exciting opportunity.
In almost all cases, taking the time to allow full healing and rehabilitation is the better choice. I’ve been fortunate to work with a few of the world’s best elite and Olympic-level gymnasts/coaches, and I can tell you that the situations where someone has to ‘push through’ for their ultimate goal are few and far between. They occur, but very very rarely. Not to mention, these decisions are often made by adults, their parents, and their medical providers as a team. With this in mind, let’s review some timelines for these various injuries.
Timeframes and Variability for Ankle & Foot Injuries
We must keep in mind that while there is great science on the healing timelines for many common ankle and foot injuries, there is still a huge variability that can occur. In the big picture, factors like age, genetics, skill level, genetics, past injury history, and more all play a role. Also, the severity and reoccurrence of the injury will make a huge difference in the overall healing timeline.
Oftentimes I will hear people compare one gymnast’s injury to another. Saying that “X” ankle injury took 4 weeks in one person, so a sort of similar “Y” injury in another person will be the same. I strongly recommend people do not do this. Even with what seems like the exact same injury, say an inversion ankle sprain, due to many factors mentioned above and more the full return to gymnastics this could be wildly different.
A grade II ankle sprain in a 12-year-old level 7 gymnast who is a bar specialist might take 4 weeks to get back to front handspring vaults, while the same type of grade II ankle sprain in a 15-year-old level 10 gymnast who is a floor/vault specialist may take 8+ weeks to get back to Yurchenko layouts. My best advice is to follow the science of healing timelines (and physician/surgeons protocols when appropriate) but use the major milestones of healing as a guide. These include swelling removal, mitigation of pain, restoration of mobility, a return to daily activities, return of full strength/power, and the ability to tolerate all advanced plyometric skills.

A useful rule of thumb to use with people is that for however long a gymnast is out of practice with their injury, it will take 2-3 times as long to return. So say someone has a mild ankle sprain that keeps them out for 2 weeks, it will likely take them 4-6 weeks more to fully return.
This being said, in my experience and based on the scientific literature, with less severe injuries like muscular strains, grade 1 sprains, and mild flare-ups of tendonitis, it could be very benign and only take 2-4 weeks to recover.
As the severity of the injury progresses, the timelines extend. Higher degree muscular strains, Grade 2 sprains, mild bone bruises, stress reactions, or more involved tendinopathies, the timeline may extend into the 4-8 week range.
Lastly, the most severe injuries occur like partial/full muscle tears, Grade 3 ligament sprains (aka tears), OCD surgeries, Achilles tendon rupture repairs, and bone fractures take substantially longer likely in the 3-6+ month range and possibly up to a year.
The 4 Phases of Rehabilitation & Goal Milestones For Recovery
When I lecture, do consulting work, or provide rehabilitation for gymnasts, I always try to outline these 4 phases general of rehabilitation. Regardless of the injury, all athletes progress through them. Some injuries move fast if they are less severe, and some move much slower if they are more severe.
Keep in mind that for me, recovery refers to fully getting back to gymnastics without physical or mental hesitancy. Being ‘cleared’ by a medical doctor from a tissue healing point of view doesn’t necessarily mean being fully ready to return to full gymnastics practice. I know and work with many amazing gymnastics-based medical providers, but I know not everyone has this luxury. This is why I try to abide by the 4 Phases of Rehabilitation. They are as follows,
1. The Acute/Subacute Phase – “Put The Fire Out”

In this phase, it’s all about damage control. In some situations, like an ankle sprain, this is more mild meaning simply having the gymnast rest for a week. It might just require some time of hard impact, elevation, basic strength/balance exercises, and using softer surfaces for a few practices.
In much more severe settings like an acutely broken ankle, this means the person needs to be immediately taken to the hospital to stabilize the fracture, get imaging done, and get a book/crutches given to them in the short term until they can see a surgeon or foot specialist. After we get through this super acute stabilization period, here are the main things I look to work on with every injury, generally in the 1-4 week range based on the injury.
Workload Reduction
This is often the most basic advice, but the hardest for gymnasts and coaches to swallow. There is no way around it, if someone has a notable foot/ankle injury they are going to need to reduce their workloads. In mild injuries, this may be 1-2 weeks on the trampoline or softer surfaces while continuing all their other nonimpact work just fine. For other more intense injuries, this may mean 4, 6, or 8+ weeks away from using their ankle or foot.
This means not only no impact but also maybe not being able to do drills or conditioning on other events because the risk of hitting or jarring their ankle is high. In some situations, there are many things gymnasts can still do in the gym including strength, flexibility, core/upper bodywork, and bars. In other situations, the risk is too high and the healing needs to be resepcted. I once had a high-level patient who ‘tried’ to do some bar releases after a bad ankle sprain. She missed her hands on a pac, hit her foot on the 8″ and was set back 6 more weeks due to reinjury.
I empathize as a former gymnast and as a current coach/PT, but. we have to be smart and use common sense. From a mental health point of view, I completely get that many gymnasts want to be in the gym, training with their friends, having fun, and doing skills they love. It can be hard to watch everyone else doing skills, routines, or competing when you are sidelined with a boot and crutches. This said it is crucial that the timeline of healing be respected here.
Even if the hours are cut by 50%, or a gymnast only goes in a few days per week to do their PT and upper body strength, that can be massive to maintain morale. Also, there is great research that by trying to maintain as much workload as possible, we may be able to get back to full gymnastics faster. Again, this is not an excuse to just ‘try’ things. I’m talking about strength. and flexibility, not tons of skill work. There have been plenty of gymnasts that we put on a combined arm/leg bike, prop their leg up on a stool next to them, and let them pedal away with just their arms and noninjured leg. This is where creative coaching plans, collaboration with medical providers, and great cultures are imperative.
Swelling/Pain Management
One of the most basic things that need to happen after an injury is preventing an excessive amount of swelling from occurring in the ankle or foot. In the last decade, there has been a big movement away from using ice to help reduce swelling, as new research suggests that it might not be the most helpful. The more favored approach now is to move the area to tolerance or move the joints around the area, to facilitate the clearance of swelling and promote the proper in/out blood flow movements.
Compression, via ace wraps or compression, is also useful here. A combination of elevation, light movement to tolerance, and compression are my go-to recommendations for swelling reduction. It can be challenging due to gravity pulling down fluid, so consistency over intensity is the key here. This tends to also help with pain, along with medication use if recommended by a medical doctor.
However, an important caveat that I will say is that we don’t want to get dogmatic and say “no ice ever”. While I have reduced ice usage by 90% or so, ice can be useful as a temporary way to help numb/reduce acute pain. So, in some situations and sometimes after big surgeries, I do use small doses of ice temporarily as a way to help manage pain. It can also be a bridge to help someone exercise more comfortably, which is the big goal.
I was once in a situation where a gymnast landed on the concrete near the floor while tumbling and fractured her heal. She was going into shock due to how painful it was. When we wanted to apply ice one medical provider said “we shouldn’t use ice, it will delay healing”. Clearly, in this situation, the ethical thing to do was to help the girl screaming in pain from not freaking out more. Some common sense is needed with applying literature. For those interested, my boss and mentor Mike Reinold has a great article on his blog to read.
Restore Basic Flexibility and Range of Motion
By reducing workloads, managing swelling, and bringing down pain, we can start to move the ankle/foot more comfortably. This allows us to help start restoring basic flexibility and range of motion. This is typically done through consistent exercise, hands-on work from a rehab provider, and weight-bearing progressions once cleared for it by a doctor. We want to restore both soft tissue flexibility and joint flexibility. We start with passive motion and then progress to active motion.
For passive motion, I like starting with 5 minutes of heat to increase blood flow, then using light massage (assisting swelling clearance and muscle relaxation) to the calf muscles, shin muscles, and bottom of the foot.
Following that, light joint glides to the ankle joints to help the up/down, and side to side motions are really useful. I also then usually passively put someone’s ankle through up, down, and sideways motions based on their injury and tolerance.
Then as a home program, I will have to use their hands to move their ankle/foot into the specific directions we are aiming to improve. I try to go for consistency over intensity, so I will give someone 10-20 repetitions of self soft tissue work, and these motion exercises multiple times throughout the day.
This helps with motion and swelling reduction. If they are able to bear weight, I will also have them go in a kneeling position and rock forward/back into a ‘toes up’ motion, pointing their knee towards their pinky toe, 10x with a 10-second hold on the last rep multiple times per day. I will also instruct athletes on some light joint mobilizations they can do safely on their own that mimic the hands-on ones that I do.
My general rule of thumb for pain levels is that during or after exercise, I don’t want someone to exceed a 3 > 10 on a pain scale, with 0 being none and 10 being severe pain. So if someone does some range of motion work, and has 2-3/10 discomfort that doesn’t get worse after or the next day, I’m generally okay with that.
Maintain/Restore Basic Strength
It’s crucial that we try to maintain as much strength as possible, and also restore baseline strength when appropriate. The active range of motion exercises is the start of this mentioned above. One of the most common ankle strength exercises done is resisted elastic band motions, going up, down, inward, and upward.
I like these, and use them, but I’ll be honest in saying that I quickly move on from them even if harder resistances are used. In my experience, I find that they are pretty easy for athletes after a while, and are a bit overused as ‘prehab’ in gyms. We want to strengthen the ankles in weight-bearing and more sport-related ways as much as possible.
I will share some videos below, but keep in mind SHIFT’s YouTube Channel has all of them, including about 500+ free exercises to check out. See more here – https://www.youtube.com/c/SHIFTMovementScienceandGymnasticsEducation/playlists
My go-to progressions after band exercises are
- Seated calf raises
- Standing calf raises
- Shin lifts
- Towel scrunches
- Toe lifts
- Arch drops.
I find these exercises can easily be loaded and progressed in a challenging way that’s appropriate to the early phase. Along with the ankle, I like to do a ton of strength work to the joints above the ankle to maintain strength. If someone can’t bear weight, things like knee extensions, hamstring curls, side plank leg lifts, side plank leg lifts, and hip extensions are great. We also use a ton of Blood Flow Restriction training in this time period, which is a great way to maintain or build strength when someone is unable to use external weights.
Return To Normal Walking
The last big goal of this acute phase is to normalize walking. For some injuries, this happens in days and does not require much progression. For other more severe injuries or surgeries, the use of a walking boot, crutches, or other weight-bearing precautions makes this occur over multiple weeks. This progression back to normal weight-bearing is important not only for mobility and strength but also because the active muscle pumping action of the lower body helps to promote blood flow in and out of the area.
When cleared, and per the guidance of medical doctors, I try to recommend that a slow weaning process occurs for weight-bearing. This helps prevent the sudden irritation of foot muscles/tendons of the injured area. To do this, I generally teach athletes to progress over the course of a week. So say they are on two crutches, we might spend start with just a few hours in the morning using one crutch but two for the rest of the day.
Then, over the week we may add 2-3 more. hours of morning one crutch time, and less afternoon two crutch time. By the end of the week, they can try a full day on one crutch. Then we do the same from one crutch to no crutches. I do a similar progression for weaning out of a boot or immobilizer if that was used.
Once the athlete has less pain, minimal swelling, good progress in flexibility returning, returning strength levels, and relatively normal walking tolerance, we progress to phase 2.
2. The Intermediate Phase – “Be A Human Again”

In this phase, generally from the 4-8 week range, the focus is very much so on strength and conditioning. The main goals are that someone can tolerate all the non gymnastics things they have to do in their day-to-day life. Climb stairs, walk all day, get to classes, lift things, and so on.
While I do still do some hands-on work and mobility here, exercise progressions really should be the main focus of this second phase. To do this we want to focus on local ankle strength, global leg/core strength, and balance or dynamic stability work.
For local strength work, this is mainly about progressing the basic exercises above. I aim to get athletes doing
- Heavier seated single leg calf raises off a 2-4″ step,
- Standing weighted single leg calf raises off a 2-4″ step
- Resisted band or dumbell shin lifts
- Bent and straight knee tip toe walks with dumbells in hand
- Single leg arch drops (possibly using a slant board)
- Squatting – Goblet box squats (can elevated heels if mobility an issue)
- Hinging – Single leg glute bridges and kettlebell deadlifts
- Split Pelvis – Split squats and sled pushing/pulling
- Single-Leg – Step-ups, step downs, single leg Romanian deadlifts
- Single leg balance holds with eyes open, then eyes closed
- Single leg balance holds while doing ball rebounds on an airex pad forward and sideways
- Split squats and step-downs on an unstable surface while getting manual perturbations from a therapist
3. The Advanced Phase – “Be An Athlete Again”

In this phase which is commonly missed or not really focused on, we are aiming to restore the basic qualities that all athletes need. Which is along with the movements above, the ability to run, jump, land, change direction, and be powerful. This sets the foundation for a smooth return to gymnastics in the next phase. Without it, it is very easy for gymnasts to not develop their full capacity and struggle with reinjury once they try to start skill work. I find that many people tend to not do this phase because oftentimes gymnasts have no pain, and feel ready to go. Take it from me though, it is worth the time and effort to go slow here and respect normal adaptation timelines. I generally find this phase occurs between the 12-16/20 week timeframes, again based on the injury severity.
First comes the need to start reintroducing plyometrics and impact work. This is often an intimidating area for gymnasts and medical providers, but if the first few phases are done well, there is typically no issue with starting to do impact work. Keep in mind for some injuries like cartilage or fractures, this will take a while and will require clearance from a doctor/surgeon. These are the exercises I use to start this
- 20 Pogo hops
- 20 In and out hops
- 20 Scissor hops
- 2 laps Jogging laps forwards and backwards
- 2 laps Skipping laps forward and sideways
- 2 laps Carioca and side shufle laps
- Vertical force – seated dumbbell jumps, box jumps, high skips, depth drops, medball slams and throws
- Horizontal force – broad jumps, forward sprinting/running progressions, and change of direction drills
These tend to be a bit more demanding, so usually I program them in sets of 2-4 repetitions of 3-5. As with the phase above, these can be built into programs and slowly progress over time until gymnasts are tolerating high power and high impact-based drills.
I also like progressing some. of the dynamic stability work. This can include unstable surface squatting/balance work, or more jumping and landing progressions. to one leg with rotational demands.
4. The Return to Sport Phase – “Be A Gymnast Again”
This is another very important, yet sometimes murky, area of gymnastics rehabilitation. While there has been great work by some researchers suggesting sports progressions, and other work to look at in baseball/tennis/golf, the reality is that gymnastics still largely has a lack of objective science-based return to sport protocols. Based on these tools and others, there are 3 main variables that I use to make return to gymnastics programs.
- Surface – soft surfaces like pit/trampoline, to medium surfaces like rod strips and using 8″ mats, to hard surfaces like spring floors or beams
- Force per skill – low impact force basics and drills, to moderate impact force skill or skill combination work, to high force power tumbling or vaulting or dismounts
- Repetitions – low repetitions per week, to moderate repetitions per week, to high repetitions per week

When I make these programs, I take the skills that a gymnast is currently performing and map them across the week. I have gymnasts do skill work 3 days per week, with 24 hours in between, while maintaining their strength program. I typically progress them every 2 weeks, making sure not to increase the surface demand, force per skill, and repetitions all at once. This typically looks like
- Weeks ½ – Soft Surface, Drills/Basics, Low Repetition volume
- Weeks ¾ – Soft/Medium Surface, Skills, Moderate Repetition volume
- Weeks ⅚ – Medium/hard, Harder skills, Moderate Skill Volume
- Week ⅞ – Hard Surfaces, Hard Skills, no > 7 reps per skill per day
Again, keep in mind that with mild injuries each phase may only take 1 week, totaling 4 weeks. In more severe injuries or those requiring surgeries, it may take 2-4 weeks for each phase, expanding the total time out to possible 8 or 16 weeks. While there are many caveats to these rehab programs, and individualization must always be applied based on the unique case, hopefully, these general guidelines can be useful.
If you want a very in depth break down of returning to impact after an injury, check out this popular YouTube video I made.
What Can Be Done To Speed Up Healing in Gymnastics Foot/Ankle Injuries?
As I mentioned, we can’t magically eliminate the natural healing timelines of tissues. But, there are many things that we can do to assist in the healing process and help optimize the body. In my experiences, these are typically less talked about as focus points. I feel that far too many people are looking for the “best exercise” or new fads in technology to try and speed up the healing process. This typically just leads to frustrations and stalled progress. Based on the literature I have reviewed and my experiences, the biggest things we can do to assist in injury recovery are
Time
As mentioned, allowing for proper timelines of healing is crucial. We want to make sure that we apply the optimal dose of loading, followed by the optimal dose of recovery, to get tissue adaptation. If we apply too much load too soon or don’t allow enough time for recovery, we can spin our wheels and run into frustrations. As literature supports, we want to shoot for the optimal dose of stress followed by the proper period of rest for the body to heal. While this will vary from tissue to tissue (tendon vs bone vs cartilage), it still applies universally.
Sleep
Getting enough sleep, and getting high-quality sleep, are both enormously important for our body’s recovery. I refer people to some great researchers like Matthew Walker and Andrew Huberman for the great information. Some of the most common tips they suggest are
- Aiming to look at morning sunlight within the first 60 minutes of waking, and trying to see evening sunsetting light
- Having consistent waking/sleeping schedules, even on weekends
- Avoiding screens or blue light 1- 2 hours prior to bed
- Sleeping in a slightly cooler room, 68 degrees F or below
- Avoiding caffeine intake 8-10 hours before bed
- Avoiding food intake 1-2 hours before bed
Proper Fueling
Tissue healing depends on having the proper fuel sources for the body to build that tissue from. It is absolutely crucial that gymnasts are getting not only enough food intake but also high-quality ingredients, for their bodies to heal. This is not my area of expertise, but I’m lucky to be friends with some expert medical providers who specialize in nutrition for gymnasts. For more information, check out Christina Anderson, Josh Eldridge, and Kerry Blair.
Compression & Active Movement To Tolerance
As outlined extensively above, there has been a movement away from icing and into promoting movement and activity to tolerance. For those looking to help speed up the recovery process, we can try to manage the swelling, motion, and blood flow as much as possible.
Static compression garments, like compression sleeves or ace wraps, can be useful. However, intermittent pneumatic compression, say in the form of mechanical dynamic compression garments like Normatec’s, has great support in the literature to restore cellular environments for recovery. While there is not extensive medical literature on ankle injuries and compression, I do try and build it into programs when appropriate.
Proper Exercise Progressions
Above all else, we have to remember that the human body senses, responds, and adapts to the appropriate dosage of load (the geeky term being mechanotransduction). The 4 phases of rehabilitation, and all the exercises I outlined above, provide the framework for how this can be done for gymnasts with ankle and foot injuries. It’s also the reason why strength and conditioning principles are so crucial. We must be using both external weight training and body weight strength training to help increase capacity, and build a robust athlete through physical preparation.
How Do We Prevent Ankle and Foot Injuries in Gymnastics?
So with all this in mind, what can we do to stay ahead of injuries? We do have many great tools we can think apply given all this information, but it is worth noting that ‘preventing’ injuries probably isn’t realistic.
For one, injuries are extremely complex with multiple factors contributing to them. Even the best science-based “prehab’ program can address all of these.
Second, gymnastics (and all sports) are just inherently risky. There will always be bumps, bruises, and accidents that happen. While I’m certainly a fan of trying as much as we can to reduce the risk of injuries, being realistic is also important. Let’s take a look at some evidence-based concepts that we can apply to reduce the risks of foot and ankle injuries.
Workload Planning, Management, & Monitoring
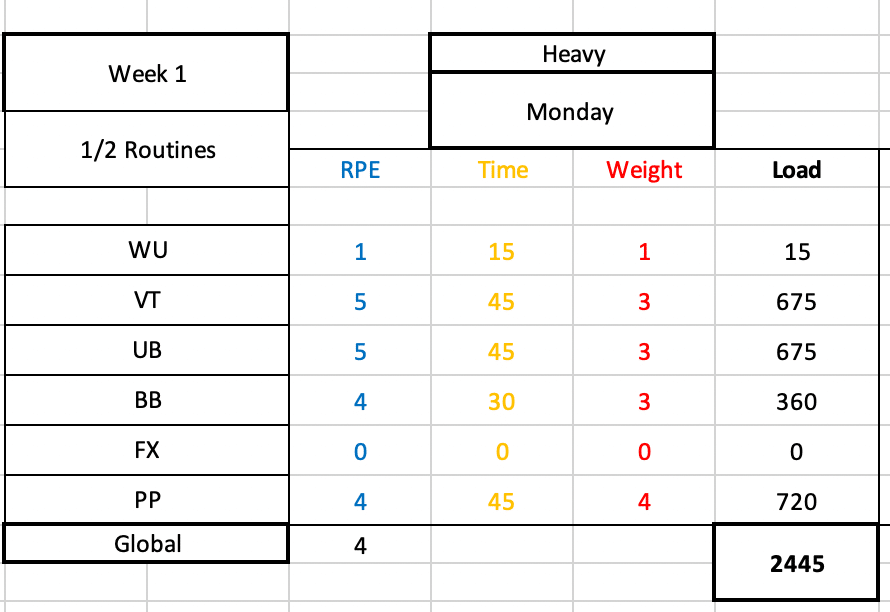
While the workload research is progressing to be less about ‘injury prevention and more about monitoring, there is great data thus far to suggest that keeping a close eye on workload can be useful.
For one, we want to make sure that we don’t subject gymnasts to rapid, unplanned, sudden spikes in impact workload. This rapid increase in load might be too much for a gymnast’s ankle/foot to handle and may contribute to elevated injury risk. This often times happens just before competition season, or when coaches might get over-excited and throw lots of new drills or plyo conditioning at gymnasts.
In another light, we also don’t want to undertrain gymnasts so that they are unprepared for the demands of gymnastics. If gymnasts are not doing an appropriate amount of skill, strength, and impact training, we may set them up for issues. Another theme in the workload research is that hard, but intelligently designed training programs, are helpful to try and reduce injury risk and increase performance.
We find the workload ‘sweet spot’ of not too much but too little, by being meticulous about the science of periodization and planning along with constant communication. We must map out the entire year, month-to-month goals, week-to-week force progressions, and daily assignments, so that we can create a progressive increase in load and back off when needed to allow recovery.
Great Strength & Conditioning Programs

This goes hand in hand with the workload concept, but formal science-based strength programs are one of the best tools that we have in helping reduce injury risk and increase performance. There is a great body of evidence suggesting that strength training, primarily with the proper usage of external weight training, is fantastic for athletes. I’m a huge fan of external weight lifting and bodyweight gymnastics being used together, in what I call ‘hybrid’ strength and conditioning programs. This is of particular importance for the lower body and foot/ankle injuries, given the forces that gymnasts experience.
Despite the overwhelming amount of evidence for the use of weight training, gymnastics culture is still largely resistant to adopting it. Many fear that it will make gymnasts ‘bulky’, lose their flexibility, or get hurt. Again, the research conflicts with this particularly when proper coaching, proper programming, and proper progression is used. For more information on this, check out this popular blog post I wrote.
Fostering Cultural Changes Around Early Specialization, Year-Round Training, and Age Guidelines
Continuing on the challenge of cultural norms, the continued focus on early specialization, year-round training, and very young gymnasts possibly being pushed too hard/too soon are huge concerns.
As with strength and conditioning, there is a massive amount of research highlighting the possible dangers of this. Both year-round training and early specialization have been associated with elevated injury risk, elevated burnout rates, and drops in long-term performance. While I do believe that there will be some lean towards earlier ages for gymnasts, particularly if they have high level goals, the tough reality is that we need to have some serious conversations about if this is beset for gymnasts’ health and long term performance.
I feel this matters most in situations like impact-based ankle/foot injuries. Doing only gymnastics from an early age, and doing it all year long, maybe subject young athletes to massive amounts of high force impact repetitions. This may create a notable risk of various injuries, and also contribute to burnout or stalled long-term performance.
Similar to this, currently are no guidelines for how many training hours per week young gymnasts of various levels should be training. How many hours per week should an 8-year-old level 6 gymnast train? What about a 13-year-old level 10? Is it ideal for the age limit of senior elite gymnastics to be 16, not 18?
I don’t have the answers to these questions. But, if we want to see actual, lasting change on the rates of ankle (and all) injuries, with higher levels of long-term performance, we must get groups of experts from all disciplines to get together and brainstorm these ideas. Particularly those around training hours, and changing our culture to not ask pre-pubertal 10-14-year-old gymnasts to be elite athletes well before they are physically or mentally ready.
Teaching Excellent Gymnastics Technique & Landing Technique

While this is not something with a ton of scientific support, it makes sense to apply the idea that a focus on excellent basics, technical foundations, and mastering proper skill progressions over multiple years is what’s best for gymnasts. During the younger years when growth and puberty are occurring, we want to help protect athletes’ bodies by teaching and using the excellent techniques. This means teaching proper running, tumbling, bounding, and dismount techniques. It also means applying the best science to proper landing techniques and making sure that the judges are not deducting when athletes land properly.
This requires gym cultures that are willing and able to invest in these more ‘boring’ sides of the sport. It also requires a culture that as a whole is willing to build an educational model where coaches are required to go through academic and mentorship to learn the best practices here. We can’t just throw a bunch of drills at coaches through online forums or lectures and expect them to go back to their gym and magically know what to do. In my opinion, I think we need a 1 year combined academic/mentorship model for anyone wanting to coach gymnastics. Then, an additional 1 year of advanced course work and mentorship for those who wish to work in the higher levels of optional, college, and elite gymnastics.
Mat Usage and Surface Monitoring
Lastly, one of the major things that we can do to help reduce the risk of ankle and foot injuries in gymnastics is by utilizing the massive amount of matting technology we have at our disposal. Various sting mats, 8″ or 12″ mats, resi pits, and other devices allow gymnasts to not only train high-level skills but also compete with buffered forces. I know that financial barriers are sometimes here, but athlete safety and longevity are by far and away from the number one priority for us.
To go along with this, we must meticulously plan the progression over the competitive year from soft to semi-firm, to hard surfaces. If people think about starting to compete in December of a year, we must look backward 3 months in advance and design slow, methodical progressions from softer to harder surfaces. As we’ve seen, jumping too fast into hard surfaces without adequate time and physical preparation will significantly increase the possible injury risk. Again, education is huge here for coaches, medical providers, strength coaches, and sports scientists to all come together and create consensus statements that will help the community.
What Do We Do If Gymnasts Ankle or Foot Injuries Aren’t Improving?
I would be denying the obvious if I didn’t admit that despite all the best practices, there are times when gymnasts’ ankle and foot injuries simply do not make progress. They take the appropriate time off, move through rehabilitation, and try to regain strength, but whenever they try to do their skills pain returns. In my experiences, here are the biggest factors to look into if someone can’t seem to get over their foot or ankle injury.
Culture Issues

This is by far and away from the biggest ‘elephant in the room’ issue that comes up when I work with gymnasts who seem to have long-lasting foot and ankle injuries. It’s crucial to make sure that the gym and community culture is not only supportive but aligned. By aligned, I mean sharing common goals.
In my experience, I find that sometimes the goals of the gymnast have changed for them to no longer want to train in a particular level of the sport, or honestly, they may not want to do gymnastics anymore. If open communication is not used, and a gymnast’s goals are not shared with parents, coaches, and medical providers, friction will result. An honest discussion about this is the first place to start if someone is struggling to get back.
Although it is less common these days, the brutal reality is that in some gyms a toxic culture exists where there is a lack of trust and athlete-centered focus. If adults are being a bit too selfish, and are not respecting someone’s injury or medical advice, they may downplay or disregard the athlete’s pain levels.
Or they may try to ‘test the waters’ on skills and go back to impact work too fast. Or, they may not be open to modifying skill profiles of gymnasts (say a less hard dismount/tumbling pass in an upcoming meet, or only doing 2 events). In some situations, gyms may not be willing to go way back to basics and correct skill techniques or get stronger as they are in season and want to rush back to competing.
When this is happening, my first recommendation is always to have a private discussion with everyone involved through the lens of empathy. Everyone likely wants the same things – for athletes, coaches, and parents to be happy and healthy. When professional discussion can occur, you can talk about the issues head-on, brainstorm solutions, and take action to change things.
If you are part of a place where someone is not open to communication or is unwilling to change, you have to ask yourself “Is this a good fit?”. Sometimes hard choices have to be made about parents, coaches, or gyms. It can be challenging, but nothing is worth sacrificing someone’s term mental or physical health.
Rehabilitation is Not Challenging Enough

Just as there can be issues with the sport and coaching side of things, there can be issues with the medical side of the fence as well. Most often, issues related to not applying the science of strength and conditioning to rehabilitation.
I find in many programs, the basic exercises that are very appropriate in the first two phases of rehabilitation never progress to advanced strength, plyometric, or power exercises. This can leave athletes short, as they are not able to rebuild their capacity. Then, once they try to go back to even basic gymnastics skills, the pain returns. Sometimes taking a step back, and really hammering strength for 4-6 weeks, is the key to getting over the hump.
In other situations, medical professionals may really lack an understanding of the sport of gymnastics. If they do not understand skill names, events, levels, and different training equipment that can be used, it might be easy to get lost. It is challenging to find medical providers who understand gymnastics, I admit this. But, thanks to the internet and many online forums, there are certainly places to develop and share this knowledge. There are also many educational platforms that can aid people in helping gymnasts more specifically.
Return To Sport Progression is Too Fast

I commonly find that the return to sports progression is too fast following ankle or foot injuries. This could be due to gymnasts not feeling pain, meet season pressure, a lack of guidance, external pressure, but the reality is that if we go too fast too soon it is very easy to flare issues up.
We have to remember that once we add in more skills or training days, we are likely adding hundreds and hundreds of impacts per week. These impacts are very high force, even when basics or soft surfaces are used. In some cases with higher levels, I find that even progressing every 2 weeks for 8 weeks might be too much. We must always respect the natural adaptation process, and be understanding when someone may hit a speed bump needing to pump the breaks a bit.
Skill Technique Not Being Corrected
This is typically more on the gymnast, but it’s crucial that skill technique and landing technique be corrected if it’s an issue. Athletes who struggle with shaping positions, basic strength, tumbling mechanics, or skill foundations may have a tough time with getting back to high-impact skills. This is typically the most common for floor, vault, and dismounts.
Following injury, the ankle and feet will. be more sensitive to short landings or high forces. If someone is throwing their head out on a floor tumbling pass causing them to land short or doesn’t understand tapping mechanics to fully rotate a dismount around, this must be corrected. Without this, problems may continue to surface over and over.
Lacking Patience with Growth and Development
This last one is really more about the entire sport of gymnastics changing their perspective on the expectations we place on children in the sport. Up until the age of 16 (or more), it is a constant uphill battle against growth and development. This is a normal part of being a human that is out of the gymnast’s control. They will grow, lose flexibility temporarily, lose strength, struggle with skills, have hormonal/mental health issues, and much more.
Gymnasts are already so hard on themselves, and if an adult is lacking compassion or is putting more pressure on them, it’s a nightmare. I see this often when a young gymnast is being asked to return back quickly after an ankle/foot injury, saying they will “miss their shot” if they don’t do _______ competition. This is a really dangerous approach to take, and has to be pushed out of our sport.
Concluding Thoughts
So that brings this absolutely monstrous, epic blog post to a close. While I highly doubt that anyone read the entire thing, my hope is that you were able to jump around to get the relevant pieces of information they needed. I will continue to update this blog post over the years as I learn more, new science emerges, and I gain more experience. As mentioned above, if you want more on the topic you can check out SHIFT’s Gymnastics Strength and Conditioning Course, our monthly membership group The Hero Lab, or our full CEU approved Gymnastics Lower Extremity course for medical providers.


If there are other issues not covered here, or things you would like to learn more about, be sure to reach out to us on social media so I can put it on my to do list!
Take care,
Dave
Dr. Dave Tilley DPT, SCS
CEO/Founder of SHIFT Movement Science
References
- Thomas RE, Thomas BC. A systematic review of injuries in gymnastics. Phys Sportsmed. 2019 Feb;47(1):96-121. doi: 10.1080/00913847.2018.1527646. Epub 2018 Oct 8. PMID: 30246587.
- Bruggemann GP., Hume PA. Biomechanics related to injury. In Handbook of Sports Medicine: Gymnastics. 2013. Wiley-Blackwell
- O’Kane JW, Levy MR, Pietila KE, Caine DJ, Schiff MA. Survey of injuries in Seattle area levels 4 to 10 female club gymnasts. Clin J Sport Med. 2011 Nov;21(6):486-92. doi: 10.1097/JSM.0b013e31822e89a8. PMID: 21959798.
- Westermann RW, Giblin M, Vaske A, Grosso K, Wolf BR. Evaluation of Men’s and Women’s Gymnastics Injuries: A 10-Year Observational Study. Sports Health. 2015 Mar;7(2):161-5. doi: 10.1177/1941738114559705. PMID: 25984262; PMCID: PMC4332645.
- Kerr ZY, Hayden R, Barr M, Klossner DA, Dompier TP. Epidemiology of National Collegiate Athletic Association Women’s Gymnastics Injuries, 2009-2010 Through 2013-2014. J Athl Train. 2015 Aug;50(8):870-8. doi: 10.4085/1062-6050-50.7.02. Epub 2015 Jul 21. PMID: 26196702; PMCID: PMC4629945.
- Paxinos O, Mitrogiannis L, Papavasiliou A, Manolarakis E, Siempenou A, Alexelis V, Karavasili A. Musculoskeletal injuries among elite artistic and rhythmic Greek gymnasts: A ten-year study of 156 elite athletes. Acta Orthop Belg. 2019 Jun;85(2):145-149. PMID: 31315004.
- Kolt GS, Kirkby RJ. Epidemiology of injury in elite and subelite female gymnasts: a comparison of retrospective and prospective findings. Br J Sports Med. 1999;33(5):312-318. doi:10.1136/bjsm.33.5.312
- Bruggemann GP., Hume PA. Biomechanics related to injury. In Handbook of Sports Medicine: Gymnastics. 2013. Wiley-Blackwell
- Sands WA. Characteristics of Gymnastics Injuries. In Jemni The Science of Gymnastics: Advanced Concepts 2018. Routledge
- Atikovic A. Kalinski SD., Cuk I. Age trends in artistic gymnastics across world championships and the Oylmpic Games from 2003 o 2016. Science of Gymnastics Journal 9(3):251-263
- Balyi I. Long-Term Athlete Development: Trainability in Childhood and Adolescence Windows of Opportunity, Optimal Trainability. Victoria: National Coaching Institute British Colombia & Advanced Training and Performance Ltd. 2004. Found at – https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.732.4200&rep=rep1&type=pdf
- Balyi I., Way R., Higgs C. Long Term Athletic Development. 2103. Human Kinetics. Champaign, IL, USA.
- Bergeron MF, Mountjoy M, Armstrong N, et al International Olympic Committee consensus statement on youth athletic development British Journal of Sports Medicine 2015;49:843-851.
- LaPrade RF, Agel J, Baker J, Brenner JS, Cordasco FA, Côté J, Engebretsen L, Feeley BT, Gould D, Hainline B, Hewett T, Jayanthi N, Kocher MS, Myer GD, Nissen CW, Philippon MJ, Provencher MT. AOSSM Early Sport Specialization Consensus Statement. Orthop J Sports Med. 2016 Apr 28;4(4):2325967116644241. doi: 10.1177/2325967116644241. PMID: 27169132; PMCID: PMC4853833.
- Myer GD, Jayanthi N, Difiori JP, et al. Sport Specialization, Part I: Does Early Sports Specialization Increase Negative Outcomes and Reduce the Opportunity for Success in Young Athletes?. Sports Health. 2015;7(5):437-442. doi:10.1177/1941738115598747
- Myer GD, Jayanthi N, DiFiori JP, et al. Sports Specialization, Part II: Alternative Solutions to Early Sport Specialization in Youth Athletes. Sports Health. 2016;8(1):65-73. doi:10.1177/1941738115614811
- Lloyd RS, Faigenbaum AD, Stone MH, Oliver JL, Jeffreys I, Moody JA, Brewer C, Pierce KC, McCambridge TM, Howard R, Herrington L, Hainline B, Micheli LJ, Jaques R, Kraemer WJ, McBride MG, Best TM, Chu DA, Alvar BA, Myer GD. Position statement on youth resistance training: the 2014 International Consensus. Br J Sports Med. 2014 Apr;48(7):498-505. doi: 10.1136/bjsports-2013-092952. Epub 2013 Sep 20. PMID: 24055781.
- Myers AM, Beam NW, Fakhoury JD. Resistance training for children and adolescents. Transl Pediatr. 2017;6(3):137-143. doi:10.21037/tp.2017.04.01
- Windt J, Gabbett TJ. How do training and competition workloads relate to injury? The workload-injury aetiology model. Br J Sports Med. 2017 Mar;51(5):428-435. doi: 10.1136/bjsports-2016-096040. Epub 2016 Jul 14. PMID: 27418321.
- Windt J, Zumbo BD, Sporer B, MacDonald K, Gabbett TJ. Why do workload spikes cause injuries, and which athletes are at higher risk? Mediators and moderators in workload-injury investigations. Br J Sports Med. 2017 Jul;51(13):993-994. doi: 10.1136/bjsports-2016-097255. Epub 2017 Mar 8. PMID: 28274916.
- DiFiori JP, Benjamin HJ, Brenner JS, Gregory A, Jayanthi N, Landry GL, Luke A. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014 Feb;48(4):287-8. doi: 10.1136/bjsports-2013-093299. PMID: 24463910.
- Ahlquist S, Cash BM, Hame SL. Associations of Early Sport Specialization and High Training Volume With Injury Rates in National Collegiate Athletic Association Division I Athletes. Orthop J Sports Med. 2020;8(3):2325967120906825. Published 2020 Mar 12. doi:10.1177/2325967120906825
- Mosher A, Fraser-Thomas J, Baker J. What Defines Early Specialization: A Systematic Review of Literature. Front Sports Act Living. 2020 Oct 27;2:596229. doi: 10.3389/fspor.2020.596229. PMID: 33345176; PMCID: PMC7739675.
- Sweeney E, Howell DR, Seehusen CN, Tilley D, Casey E. Health outcomes among former female collegiate gymnasts: the influence of sport specialization, concussion, and disordered eating. Phys Sportsmed. 2021 Nov;49(4):438-444. doi: 10.1080/00913847.2020.1850150. Epub 2020 Nov 23. PMID: 33186080.
- Zaremski JL, Zeppieri G Jr, Tripp BL. Sport Specialization and Overuse Injuries in Adolescent Throwing Athletes: A Narrative Review. J Athl Train. 2019;54(10):1030-1039. doi:10.4085/1062-6050-333-18
- Post EG, Rosenthal MD, Pennock AT, Rauh MJ. Prevalence and Consequences of Sport Specialization Among Little League Baseball Players. Sports Health. 2021 May-Jun;13(3):223-229. doi: 10.1177/1941738120970956. Epub 2021 Feb 3. PMID: 33530863; PMCID: PMC8083145.
- Aicale R, Tarantino D, Maffulli N. Overuse injuries in sport: a comprehensive overview. J Orthop Surg Res. 2018;13(1):309. Published 2018 Dec 5. doi:10.1186/s13018-018-1017-5
- Bell DR, Post EG, Biese K, Bay C, Valovich McLeod T. Sport Specialization and Risk of Overuse Injuries: A Systematic Review With Meta-analysis. Pediatrics. 2018 Sep;142(3):e20180657. doi: 10.1542/peds.2018-0657. Epub 2018 Aug 22. PMID: 30135085.
- Evans JW. Periodized Resistance Training for Enhancing Skeletal Muscle Hypertrophy and Strength: A Mini-Review. Front Physiol. 2019 Jan 23;10:13. doi: 10.3389/fphys.2019.00013. PMID: 30728780; PMCID: PMC6351492.
- Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014 Jun;48(11):871-7. doi: 10.1136/bjsports-2013-092538. Epub 2013 Oct 7. PMID: 24100287.
- Webster KE, Hewett TE. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res. 2018 Oct;36(10):2696-2708. doi: 10.1002/jor.24043. Epub 2018 Jun 13. PMID: 29737024.
- Lloyd RS, Faigenbaum AD, Stone MH, Oliver JL, Jeffreys I, Moody JA, Brewer C, Pierce KC, McCambridge TM, Howard R, Herrington L, Hainline B, Micheli LJ, Jaques R, Kraemer WJ, McBride MG, Best TM, Chu DA, Alvar BA, Myer GD. Position statement on youth resistance training: the 2014 International Consensus. Br J Sports Med. 2014 Apr;48(7):498-505. doi: 10.1136/bjsports-2013-092952. Epub 2013 Sep 20. PMID: 24055781.
- Dahab KS, McCambridge TM. Strength training in children and adolescents: raising the bar for young athletes? Sports Health. 2009 May;1(3):223-6. doi: 10.1177/1941738109334215. PMID: 23015875; PMCID: PMC3445252.
- Zwolski C, Quatman-Yates C, Paterno MV. Resistance Training in Youth: Laying the Foundation for Injury Prevention and Physical Literacy. Sports Health. 2017;9(5):436-443. doi:10.1177/1941738117704153
- Peitz M, Behringer M, Granacher U. A systematic review on the effects of resistance and plyometric training on physical fitness in youth- What do comparative studies tell us? PLoS One. 2018 Oct 10;13(10):e0205525. doi: 10.1371/journal.pone.0205525. Erratum in: PLoS One. 2018 Nov 14;13(11):e0207641. PMID: 30304033; PMCID: PMC6179270.
- Webster KE, Hewett TE. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res. 2018 Oct;36(10):2696-2708. doi: 10.1002/jor.24043. Epub 2018 Jun 13. PMID: 29737024.
- Mason-Mackay AR, Whatman C, Reid D. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: A systematic review. J Sci Med Sport. 2017 May;20(5):451-458. doi: 10.1016/j.jsams.2015.06.006. Epub 2015 Jun 15. PMID: 26117159.
- Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder?. Br J Sports Med. 2016;50(5):273-280. doi:10.1136/bjsports-2015-095788
- Gabbett TJ, Nassis GP, Oetter E, Pretorius J, Johnston N, Medina D, Rodas G, Myslinski T, Howells D, Beard A, Ryan A. The athlete monitoring cycle: a practical guide to interpreting and applying training monitoring data. Br J Sports Med. 2017 Oct;51(20):1451-1452. doi: 10.1136/bjsports-2016-097298. Epub 2017 Jun 23. PMID: 28646100.
- Debien PB, Timoteo TF, Gabbett TJ, Bara Filho MG. Training-Load Management in Rhythmic Gymnastics: Practices and Perceptions of Coaches, Medical Staff, and Gymnasts. Int J Sports Physiol Perform. 2022 Jan 11:1-11. doi: 10.1123/ijspp.2021-0279. Epub ahead of print. PMID: 35016155.
- Thomas E, Bianco A, Paoli A, Palma A. The Relation Between Stretching Typology and Stretching Duration: The Effects on Range of Motion. Int J Sports Med. 2018 Apr;39(4):243-254. doi: 10.1055/s-0044-101146. Epub 2018 Mar 5. PMID: 29506306.
- O’Sullivan K, McAuliffe S, Deburca N. The effects of eccentric training on lower limb flexibility: a systematic review. Br J Sports Med. 2012 Sep;46(12):838-45. doi: 10.1136/bjsports-2011-090835. Epub 2012 Apr 20. PMID: 22522590.
- Hernández-Díaz C, Saavedra MÁ, Navarro-Zarza JE, Canoso JJ, Villaseñor-Ovies P, Vargas A, Kalish RA. Clinical anatomy of the ankle and foot. Reumatol Clin. 2012 Dec-2013 Jan;8 Suppl 2:46-52. doi: 10.1016/j.reuma.2012.10.005. Epub 2012 Dec 8. PMID: 23228530.
- Ficke J, Byerly DW. Anatomy, Bony Pelvis and Lower Limb, Foot. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546698/
- Chiodo CP. Understanding the Anatomy and Biomechanics of Ankle Tendons. Foot Ankle Clin. 2017 Dec;22(4):657-664. doi: 10.1016/j.fcl.2017.07.001. Epub 2017 Sep 19. PMID: 29078820.
- Melanson SW, Shuman VL. Acute Ankle Sprain. [Updated 2021 Jul 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459212/
- Martin RL, Davenport TE, Fraser JJ, Sawdon-Bea J, Carcia CR, Carroll LA, Kivlan BR, Carreira D. Ankle Stability and Movement Coordination Impairments: Lateral Ankle Ligament Sprains Revision 2021. J Orthop Sports Phys Ther. 2021 Apr;51(4):CPG1-CPG80. doi: 10.2519/jospt.2021.0302. PMID: 33789434.
- Prakash AA. Epidemiology of High Ankle Sprains: A Systematic Review. Foot Ankle Spec. 2020 Oct;13(5):420-430. doi: 10.1177/1938640020916266. PMID: 32924583.
- Williams GN, Allen EJ. Rehabilitation of syndesmotic (high) ankle sprains. Sports Health. 2010;2(6):460-470. doi:10.1177/1941738110384573
- Berman Z, Tafur M, Ahmed SS, Huang BK, Chang EY. Ankle impingement syndromes: an imaging review. Br J Radiol. 2017;90(1070):20160735. doi:10.1259/bjr.20160735
- Berberian WS, Hecht PJ, Wapner KL, DiVerniero R. Morphology of tibiotalar osteophytes in anterior ankle impingement. Foot Ankle Int. 2001 Apr;22(4):313-7. doi: 10.1177/107110070102200407. PMID: 11354444.
- Naumetz VA, Schweigel JF. Osteocartilagenous lesions of the talar dome. J Trauma. 1980 Nov;20(11):924-7. doi: 10.1097/00005373-198011000-00002. PMID: 7431446.
- Arnold A, Thigpen CA, Beattie PF, Kissenberth MJ, Shanley E. Overuse Physeal Injuries in Youth Athletes. Sports Health. 2017;9(2):139-147. doi:10.1177/1941738117690847
- Smith JM, Varacallo M. Sever Disease. 2021 Jul 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 28722957.
- Forrester RA, Eyre-Brook AI, Mannan K. Iselin’s Disease: A Systematic Review. J Foot Ankle Surg. 2017 Sep-Oct;56(5):1065-1069. doi: 10.1053/j.jfas.2017.04.030. PMID: 28842092.
- Cook JL, Purdam CR Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy British Journal of Sports Medicine 2009;43:409-416.
- Rees JD, Maffulli N, Cook J. Management of Tendinopathy. The American Journal of Sports Medicine. 2009;37(9):1855-1867. doi:1177/0363546508324283
- Cardoso TB, Pizzari T, Kinsella R, Hope D, Cook JL. Current trends in tendinopathy management. Best Pract Res Clin Rheumatol. 2019 Feb;33(1):122-140. doi: 10.1016/j.berh.2019.02.001. Epub 2019 Mar 8. PMID: 31431267.
- Martin RL, Chimenti R, Cuddeford T, Houck J, Matheson JW, McDonough CM, Paulseth S, Wukich DK, Carcia CR. Achilles Pain, Stiffness, and Muscle Power Deficits: Midportion Achilles Tendinopathy Revision 2018. J Orthop Sports Phys Ther. 2018 May;48(5):A1-A38. doi: 10.2519/jospt.2018.0302. PMID: 29712543.
- Li HY, Hua YH. Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. Biomed Res Int. 2016;2016:6492597. doi:10.1155/2016/6492597
- Ling SK, Lui TH. Posterior Tibial Tendon Dysfunction: An Overview. Open Orthop J. 2017 Jul 31;11:714-723. doi: 10.2174/1874325001711010714. PMID: 28979585; PMCID: PMC5620404.
- Walt J, Massey P. Peroneal Tendon Syndromes. [Updated 2021 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544354/
- Davda K, Malhotra K, O’Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT Open Rev. 2017;2(6):281-292. Published 2017 Jun 22. doi:10.1302/2058-5241.2.160047
- Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM; American Physical Therapy Association. Heel pain-plantar fasciitis: revision 2014. J Orthop Sports Phys Ther. 2014 Nov;44(11):A1-33. doi: 10.2519/jospt.2014.0303. PMID: 25361863.
- Debus F, Eschbach D, Ruchholtz S, Peterlein CD. Rupture of plantar fascia: Current standard of therapy: A systematic literature review. Foot Ankle Surg. 2020 Jun;26(4):358-362. doi: 10.1016/j.fas.2019.05.006. Epub 2019 May 14. PMID: 31176530.
- McClure CJ, Oh R. Medial Tibial Stress Syndrome. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538479/
- Winters M. The diagnosis and management of medial tibial stress syndrome : An evidence update. Unfallchirurg. 2020 Jan;123(Suppl 1):15-19. English. doi: 10.1007/s00113-019-0667-z. PMID: 31098646.
- Franklyn M, Oakes B. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop. 2015;6(8):577-589. Published 2015 Sep 18. doi:10.5312/wjo.v6.i8.577
- Bica D, Sprouse RA, Armen J. Diagnosis and Management of Common Foot Fractures. Am Fam Physician. 2016 Feb 1;93(3):183-91. PMID: 26926612.
- Menéndez C, Batalla L, Prieto A, Rodríguez MÁ, Crespo I, Olmedillas H. Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review. Int J Environ Res Public Health. 2020;17(20):7457. Published 2020 Oct 13. doi:10.3390/ijerph17207457
- Torg JS, Moyer J, Gaughan JP, Boden BP. Management of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010 May;38(5):1048-53. doi: 10.1177/0363546509355408. Epub 2010 Mar 2. PMID: 20197494.
- Moracia-Ochagavía I, Rodríguez-Merchán EC. Lisfranc fracture-dislocations: current management. EFORT Open Rev. 2019 Jul 2;4(7):430-444. doi: 10.1302/2058-5241.4.180076. PMID: 31423327; PMCID: PMC6667981.
- Vuurberg G, Hoorntje A, Wink LM, van der Doelen BFW, van den Bekerom MP, Dekker R, van Dijk CN, Krips R, Loogman MCM, Ridderikhof ML, Smithuis FF, Stufkens SAS, Verhagen EALM, de Bie RA, Kerkhoffs GMMJ. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018 Aug;52(15):956. doi: 10.1136/bjsports-2017-098106. Epub 2018 Mar 7. PMID: 29514819.
- Dubois B, Esculier JF. Soft-tissue injuries simply need PEACE and LOVE. Br J Sports Med. 2020 Jan;54(2):72-73. doi: 10.1136/bjsports-2019-101253. Epub 2019 Aug 3. PMID: 31377722.
- Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle Int. 2000 Feb;21(2):119-26. doi: 10.1177/107110070002100205. PMID: 10694023.
- Reinold MM, Wilk KE, Reed J, Crenshaw K, Andrews JR. Interval sport programs: guidelines for baseball, tennis, and golf. J Orthop Sports Phys Ther. 2002 Jun;32(6):293-8. doi: 10.2519/jospt.2002.32.6.293. PMID: 12061709.
- Watson AM. Sleep and Athletic Performance. Curr Sports Med Rep. 2017 Nov/Dec;16(6):413-418. doi: 10.1249/JSR.0000000000000418. PMID: 29135639.
- Beelen M, Burke LM, Gibala MJ, van Loon L JC. Nutritional strategies to promote postexercise recovery. Int J Sport Nutr Exerc Metab. 2010 Dec;20(6):515-32. doi: 10.1123/ijsnem.20.6.515. PMID: 21116024.
- Sands WA, McNeal JR, Murray SR, Stone MH. Dynamic Compression Enhances Pressure-to-Pain Threshold in Elite Athlete Recovery: Exploratory Study. J Strength Cond Res. 2015 May;29(5):1263-72. doi: 10.1519/JSC.0000000000000412. PMID: 24531439